From the journals: JLR
The role of lipids in COVID-19. The plasma lipidome: Who contributes what? Read about papers on these topics recently published in the Journal of Lipid Research.
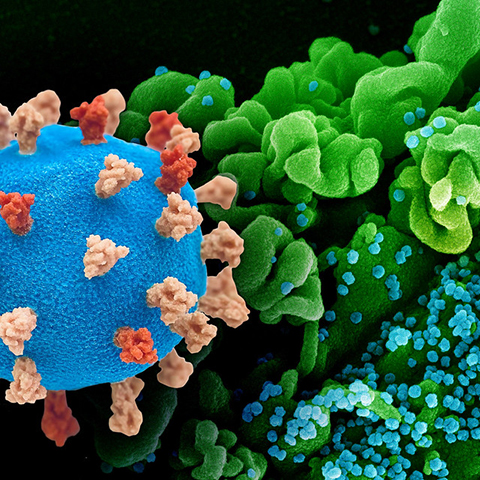
The role of lipids in COVID-19
A surface glycoprotein on the SARS-CoV-2 virus known as the spike protein mediates interaction with surface receptors in the host cell and facilitates viral entry and propagation, which is crucial for COVID-19 infection to develop. Once inside, SARS-CoV-2 hijacks the cellular machinery required for its own replication. The newly formed viral spike proteins are the target of modifications including the covalent addition of fatty acids to cysteines of the protein aminoacidic sequence. This process is called S-acylation.
Almost three years into the worldwide COVID-19 pandemic, researchers are still learning about mechanisms of viral entry and propagation. Among them are Katrina Mekhail and Minhyoung Lee at the University of Toronto and Michael Sugiyama at Ryerson University (now Toronto Metropolitan University). Along with collaborators, they examined the role of spike protein S-acylation on human and monkey epithelial cells infected with SARS-CoV-2. Their findings were recently published in the Journal of Lipid Research.
The authors showed that S-acylation of the spike protein with palmitate, a 16 carbon–long fatty acid, was mediated by ZDHHC5 and other ZDHHC enzymes and was required for viral membrane-to-cell membrane fusion and virion spread in cell culture. They also found that other fatty acids, such as myristate and stearate, can be used for viral protein acylation by different enzymes.
To see how limiting endogenous fatty acid availability affects spike protein acylation and viral propagation, the authors used the drug TVB-3166 to block fatty acid synthase enzyme in cultured human cells and mice infected with coronaviruses that cause a respiratory illness similar to COVID-19. Inhibition of fatty acid synthesis reduced viral spread and clinical symptoms and improved survival.
The plasma lipidome: Who contributes what?
More than 500 lipids circulate in the human blood, constituting what is known as the plasma lipidome. They serve as fuel to sustain cellular processes and act as signals as organs communicate. When the lipidome is altered by overeating, fasting, Type 2 diabetes or cardiovascular diseases, it becomes a useful diagnostic marker.
Various organs produce, secrete and take up lipids into and from the circulating blood to create the lipidome signature. However, we do not fully understand which organ contributes what under various physiological and pathological conditions.
In a recent article in the Journal of Lipid Research, Raghav Jain and colleagues from the University of Wisconsin–Madison and the University of Iowa describe how they exposed mice to low temperatures, which can rapidly induce lipid metabolism remodeling, and tracked over 1,000 species of lipids in plasma and in nine types of tissue, including cardiac and skeletal muscles, white and brown adipose, liver, and intestine.
When exposed to the cold, the white adipose tissue secreted free fatty acids into the blood, which then were taken by the liver. Here, fatty acyl chains were conjugated with L-carnitine to produce acylcarnitines, a lipid class that readily enters the mitochondria for energy production. In the cold-exposed mice, acylcarnitines served as fuel for the brown adipose tissue during thermogenesis. Furthermore, the authors found that the intestine was a novel site for uptake of acylcarnitines and that the kidneys contributed to their circulating pool.
This study provides lipid signatures for plasma and tissues and correlates them using a computational tool to predict tissue-specific contributions during metabolic stress. This could be important to understand how diseases change lipid metabolism.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

