World Heart Day 2021
To “lie at the heart of something” is to be at the central or most crucial part of something. If you think of the heart of the United States, it may be reasonable to think of Washington, D.C. Our nation’s capital is the seat of our federal government, where major decisions are made about our democracy and our lives.
It is a place people from all over the country rely on for action, come to protest in, and send their elected officials in an effort to have their voices heard. It is a place that is structured to house the official workplaces of the three branches of our government — the legislative branch (U.S. Capitol), the executive branch (the White House) and the judicial branch (the U.S. Supreme Court). It is also a place of employment for a workforce of more than 700,000 people, a large percentage of whom reside outside of the D.C. borders and within the Washington metropolitan area.
To put it simply, the successful function of Washington, D.C., relies on the galvanization of ideas into action, the maintenance of governmental structure, and the constant influx and efflux of American citizens.
In a similar sense, the successful function of the heart (as in the literal organ) relies on electrical activity to turn signals into action, the maintenance of its muscles and valves, and the circuitous movement of blood in and out of its vessels. We may summarize these three categories into electrical, structural and circulatory systems.
When there are problems with any one of these functioning areas, the results can be either mildly irritating or utterly catastrophic. In the Washington, D.C., example, if there is a failure to pass funding or legislation, there may be government shutdowns. If governmental buildings experience insurrections, elected officials’ lives may be at risk. And if there is traffic (“congestion,” if you will) there may be a general hold on productivity from the daily workforce.
Just as much as D.C. relies on power-driven movements, structural soundness and rhythmic interchanges, so too does the heart. If any aspect of the heart’s electrical, structural or vascular systems becomes disorderly, unorganized or impaired, the entire heart can fail, with the body soon to follow.
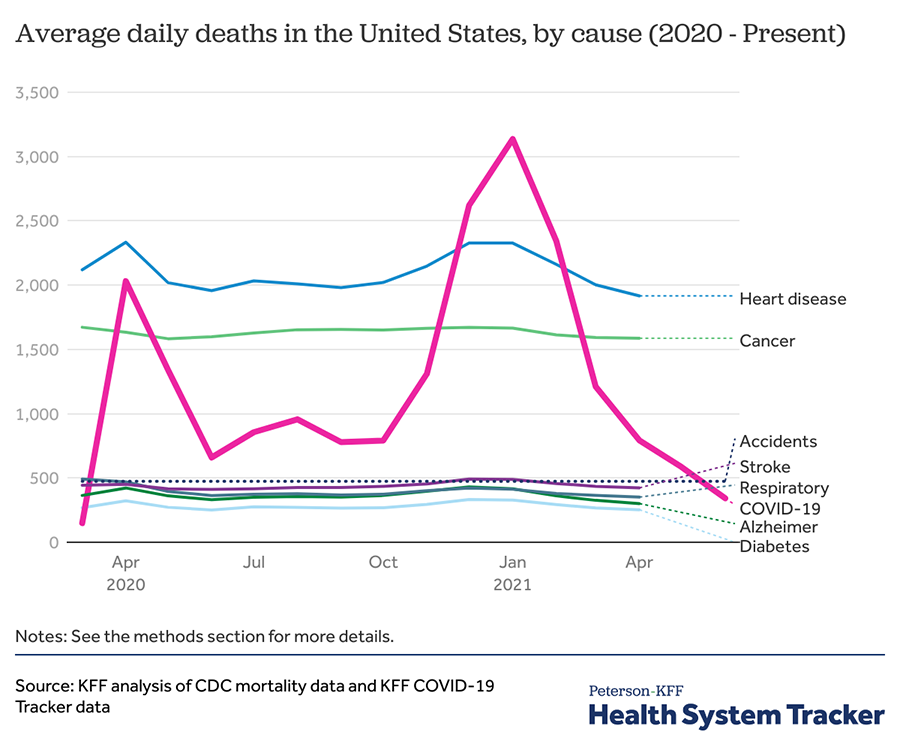
In recognition of World Heart Day, a global campaign established in 1999 by the World Heart Federation and the World Health Organization, this article seeks to cover the concepts of cardiovascular disease that has made it persist as the leading cause of death worldwide. (Note: Though heart disease has been recognized as the leading cause of death worldwide for the past 80 years, COVID-19 was the leading cause of death in the United States between December 2020 and February 2021. As of March 2021, heart disease once again topped the charts as the leading killer in the United States.)
In addition to providing information on the different types of cardiac disorders, this article provides suggestions for actions to prevent and control cardiovascular disease and shares new insights from research published in American Society for Biochemistry and Molecular Biology journals. This is not meant to be a comprehensive article but rather a showcase of promising preventative and treatment measures.
Electrical heart diseases: Faulty wiring
Electrical heart diseases are responsible for a large number of sudden, unexpected deaths. Like clocks, our hearts rely on electricity to produce rhythmic movements over time. Just as a clock ticks 60 seconds per minute, the resting heart rate typically is 60 beats per minute, each beat ejecting oxygenated blood into the body. Unlike a clock, though, a healthy beating heart can adjust its activity up to 120 beats per minute under normal conditions.
There is a wide range of heart rates that fall within the normal window for healthy hearts, and this is to allow the body to adjust its circulation rate of oxygenated blood to keep up with the body’s metabolic demands. Heart rates fluctuate based on situation. During sleep, resting heart rates are low because our body processes slow down. During periods of exercise, stress or excitement, heart rates are high because our body processes speed up. Various other factors such as temperature, body size and caffeine also can affect heart rate.
The rhythmic production of these electrical signals begins in the upper right chamber of the heart and propagates down into the lower chambers. With each beat, mechanical contractions occur and force blood out into the body’s circulatory system. However, for a variety of reasons, sometimes these electrical activities can go haywire. In these situations, either the electrical signals do not generate properly (i.e., rhythm disorders) or the electrical signals do not travel properly (i.e., conduction disorders) or both.
Rhythm disorders
When heart rates deviate outside of the normal rhythmic range, the heart experiences what is called an arrhythmia. Generally, a heart rate lower than 60 beats per minute is known as bradycardia, and a heart rate higher than 100 beats per minute is known as tachycardia. If these events are rhythmic (meaning the beat-to-beat rate is consistent over a period of time), the body is simply experiencing an exceedingly slow or fast metronome. However, if these events are abnormal or become dyssynchronous, the outcomes can be dangerous and potentially lethal.
When rhythmic dyssynchrony occurs in the atria (the two upper chambers of the heart), this may be only bothersome or uncomfortable. When rhythmic dyssynchrony occurs in the ventricles (the two lower chambers of the heart), the situation may be life-threatening. The ventricles are responsible for simultaneously pushing deoxygenated blood out into the lungs and oxygenated blood out into the body in a matter of milliseconds. If the ventricles do not electrically excite at the consistent rhythm that is set by the heart’s natural pacemaker (also thought of as the metronome), they can instead “quiver” to such an extent that blood cannot be pumped adequately and the body cannot receive the oxygen it needs to function. This quivering type of arrhythmia is known as ventricular fibrillation. Ventricular fibrillation events need to be stopped quickly. If sustained for more than a few minutes, these episodes can lower blood pressure substantially and cause cardiac arrest or even death.
Research highlight: Caffeine and heart disease
Ryanodine receptors, or RyRs, are ion channels that mediate the release of Ca2+ from the sarcoplasmic reticulum/endoplasmic reticulum and are an essential component of the excitation–contraction coupling in hearts. Mutations of RYR2 can increase its sensitivity to caffeine activation and have been linked to the development of heart diseases such as catecholaminergic polymorphic ventricular tachycardia and arrhythmogenic right ventricular cardiomyopathy type 2. In a recent study published in the Journal of Biological Chemistry, Wenting Guo and colleagues from the University of Calgary investigated the molecular mechanisms of four disease-associated C-terminal domain mutations and found that these mutations reduced the activation threshold of SOICR and increased the sensitivity of RYR2 to caffeine activation.
Conduction disorders
In addition to problems with heart rate dyssynchrony, problems can arise when there is a so-called “short in the circuit.” Two common examples of conduction system disorders are bundle branch block, or BBB, and total heart block.
BBB is a disorder with the bundle branches — the specialized strings of cells that line the inner walls of the ventricles. Under normal conditions, bundle branches propagate electrical signals to spark healthy and rhythmic mechanical pumping. In a conduction disorder, a block in either one of the two bundle branches can lead to electrical dyssynchrony and trigger a ventricular arrhythmia.
Like BBB, total heart block involves a blockage of conduction system, but the blockage occurs at a crucial junction in the heart — a place called the atrioventricular node. The atrioventricular node is a specialized group of cells that sits between the upper and lower chambers of the heart, serving as an electrical moderator to give the ventricles adequate time to receive blood from the atria. The severity of total heart block can be broken down in tiers.
-
First-degree heart block is the least serious. Here, electrical impulses pass through the AVN, but they move more slowly than normal. This type of heart block may not come with any noticeable systems but still can be seen in ECG scans.
-
Second-degree heart block is more severe. Here, electrical impulses pass through the atrioventricular node as well, but some beats intermittently are blocked. These occasional dropped beats can manifest as heart palpitations, chest pain or fainting.
-
Lastly, third-degree heart block occurs when the electrical signals through the atrioventricular node are blocked completely. This is the most serious form of total heart block. The heart beat will become irregular and unreliable, and if left untreated, third-degree heart block can lead to cardiac arrest.
Structural heart diseases: Faulty mechanics
Structural heart diseases are defects or disorders that affect the heart’s overall anatomy. These can occur in the walls, muscles or valves and can be inherited (i.e., present from birth) or acquired (i.e., developed over time). More than 10% of adults 75 years and older live with acquired structural heart disease.
Cardiomyopathy is the general term used to describe stiff or enlarged chamber walls. It results in inefficient blood circulation and can weaken the heart muscle over time. Cardiac amyloidosis is a specific disorder of the heart muscle in which protein deposits called amyloids infiltrate tissues. This type of disorder can cause excessive buildup of fluid in the body, which can lead to shortness of breath or swelling of the legs and abdomen.
Research highlight: Quantitative proteomics provide new insights into structural heart disease
Nora Linscheid from the University of Copenhagen, in collaboration with colleagues from NYU School of Medicine, recently published a comprehensive study in the journal Molecular & Cellular Proteomics on cardiac protein expression from human samples collected in vivo. Biopsy samples of the four cardiac chambers were collected from patients who had mitral valve prolapse and dilated left atria with no history of atrial fibrillation. Using high-resolution mass spectrometry techniques, this study provides insights into the first human proteome of dilated left atria in a nonatrial fibrillation state and showed that increased levels of proteins previously associated with sustained atrial fibrillation are not enough to generate the disease state. Such identification of chamber-specific differences may lead the way to the future development of chamber-targeted therapeutic strategies.
Structural heart disease occurring in the valves is another problem. In a healthy heart, there are four valves (mitral, tricuspid, aortic and pulmonary), which open and close smoothly to allow blood to pass through. Like doors of a house or bridges to an island, these valves must function properly to keep things moving. If these doors are rusty or stiff, flow may be compromised. Stiff valves are called stenosis. Valves that permit blood flow in the wrong direction are called regurgitant. Leaflet tears, calcification and atheroma (fatty deposits) are other conditions that also can affect the function of valves.
Vascular heart diseases: Faulty flow
Vascular heart diseases may be the type of heart failure you are most familiar with. Know someone with a stent? Vascular heart disease. Know someone who has had coronary artery bypass graft surgery? Vascular heart disease. This type of heart disease encompasses any condition that affects blood vessels of the heart. They are common and can be serious.
Examples of vascular heart diseases include atherosclerosis (plaque buildup inside arteries), coronary artery disease (blockage of an artery) and aortic aneurysms (ballooning of the aortic walls). In all conditions, healthy blood flow may be compromised. If left untreated, the severity of these diseases can increase significantly and lead to heart attacks or sudden death. Some signs of vascular heart disease include chest pain, fainting, dizziness, fatigue, loss of responsiveness, abnormal breathing, shortness of breath, loss of consciousness and kidney dysfunction.
Research highlight: Plasma proteins can be vasculoprotective
Plasma total cholesterol and triglyceride levels are known to be twice as high in hibernating brown bears as in healthy humans, yet adult bears display no signs of early-stage atherosclerosis development. In the Journal of Lipid Research, Matteo Pedrelli and colleagues from the Karolinska Institutet in Sweden investigated the vasculoprotective properties of plasma lipoproteins from brown bears. They found that the atheroprotective and vasculoprotective mechanisms of the bear lipoprotein profile seem to be driven by composition- and structure-modulated functions. Specifically, atherogenesis can be modulated by the association of LDL with arterial proteoglycans and the capacity of plasma to remove cholesterol from extrahepatic cells.
Causes and treatments
Though there are many types of heart diseases and the nature of these diseases varies widely, underlying causes are often the same. Some of the most common causes of heart disease include:
-
Genetics.
-
Smoking.
-
Alcohol use.
-
Poor diet.
-
Drugs.
-
Age.
-
Stress.
-
Physical inactivity.
-
High blood pressure.
-
High cholesterol.
Preventative measures and treatments
Fortunately, according to the Centers for Disease Control and Prevention, the majority of heart diseases can be prevented through healthy lifestyles and appropriate medical intervention.
In choosing a healthy lifestyle, it is recommended to eat healthy foods and choose healthy drinks. Low-sodium diets and limited alcohol use can help you maintain low blood pressures. High-fiber foods and foods low in saturated and trans fats can help prevent high cholesterol.
Also, it is suggested to maintain a healthy weight, get regular physical activity and avoid smoking. High body weights can put stress on your heart and block blood vessels from adequate circulation, but physical activity can help you maintain a healthy weight and lower your blood pressure, blood cholesterol and blood sugar levels.
By taking charge of health care measures, you can take preemptive steps to lower your risk of heart disease. Examples of being proactive in this sense include checking your cholesterol every four to six years, controlling your blood pressure through lifestyle changes, managing diabetes if necessary, taking medicines as directed and working with your health care team if you have any questions.
Research highlight: Interactions of diet and exercise in a mouse model
High-fat diets combined with low exercise contribute to the obesity burden in humans. Aerobic exercise is known to provide metabolic benefits, but researchers from the University of Sydney in New South Wales, Australia, wanted to explore how aerobic exercise specifically serves to prevent or treat high-fat diet–induced phenotypes at the molecular level. Sergio F. Martinez–Huenchullan and colleagues recently published a report in the journal Molecular & Cellular Proteomics studying the plasma proteome in mice. They identified that while the type of aerobic exercise does not seem to have a large effect on the outcome, long periods of high-fat diet have more deleterious effects, and aerobic exercise can revert the significant physiological changes associated with high-fat diets.
In addition to lifestyle changes, the World Health Organization asserts that heart disease across the world can be managed through proper health coverage.
-
Hypertension programs, when implemented efficiently, can reduce the incidence of vascular disorders such as coronary artery disease and stroke.
-
Access to proper medication can mitigate and treat electrical disorders of the heart. Basic medicines such as aspirin, beta-blockers, angiotensin-converting enzyme inhibitors and statins treat numerous forms of heart disease and should be made available throughout the world.
-
Access to appropriate technology is also important. Implantable cardiac defibrillators, permanent pacemakers and left ventricular assist devices are imperative to treat some of the most severe diseases and restore proper blood flow.
-
Minimally invasive surgical operations such as coronary artery bypass grafting, valve repair/replacement, radiofrequency ablation, balloon angioplasty and stent placement also can be life-saving options for those suffering from negative symptoms.
-
Finally, heart transplantation is a viable option for those with end-stage heart failure.
To ensure worldwide access to the myriad life-saving procedures, however, investments in strengthening health systems are imperative for reducing the incidence of this global killer.
Research highlight: Mechanisms of benzopyran as an anti-arrhythmic drug
In a recent paper published in the Journal of Biological Chemistry, Meng Cui and colleagues from Northeastern University investigated the mechanisms of action for benzopyran derivatives — promising candidates for anti-arrhythmic drugs. Using homology modeling, molecular docking and molecular dynamics simulations, the researchers characterized the compound Benzopyran-G1 and reported that it selectively inhibits the Kir3.1 (GIRK1 or G1) subunit of the KACh channel. These results may open the doors to future discoveries of novel selective IKACh channel blockers to treat atrial fibrillation with minimal side effects.
Advocacy and governmental action
This year, the global campaign for World Heart Day is based on three key pillars: equity, prevention and community. The campaign website asks the world to #UseHeart to overcome this expansive healthcare crisis and to “use your knowledge, compassion and influence to make sure you, your loved ones and the communities you’re part of have the best chance to live heart-healthy lives.”
I would like to take a moment here and hark back to the introductory analogy of this paper. I chose Washington, D.C., as an example because, in addition to being the heart of our country, it can play a vital role in mitigating heart disease in the United States and beyond.
Proper policy measures can save lives. By reducing risk factors such as tobacco use, unhealthy diets and physical inactivity, our government can help prevent at least 80% of the premature deaths from heart disease and stroke in our country.
Greater access to healthy foods in low-income neighborhoods and improved measures for reaching environmental justice can have far-reaching effects, including improved eating habits, more vibrant communities and fewer deaths.
The responsibility for curbing heart disease does not solely have to lie with the individual. More scientific research in heart failure mechanisms can lead to better understandings of the disease and improve treatment modalities. More awareness of the risks of tobacco can prevent unnecessary heart disease.
As a citizen, you can call on your local representatives to help solve this health crisis. You can educate your neighbors on heart-healthy foods. You can join or start a local exercise group. And you can make sure you and your loved ones know you have both a chance for and a right to heart-healthy futures.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.