Unraveling amyloidosis, a misunderstood disorder
Amyloidosis was first described in 1639, but all these centuries later it remains not well known to the public or health professionals. It is a rare and multifaceted disease with grave risks worsened by delayed diagnosis.
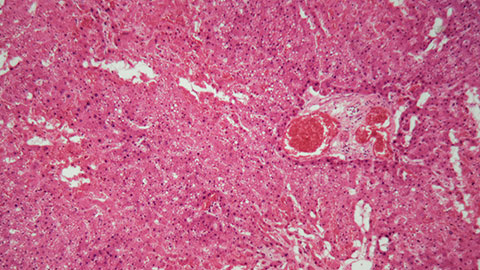
Amyloidosis occurs when amyloid proteins form clumps in tissues and organs, disrupting their normal structures and functions. It most frequently affects the kidneys, heart, liver, nervous system and gastrointestinal tract. It can also affect more than one organ at the same time. The symptoms and severity of the disease depend on which organs and tissues are affected.
Amyloidosis may be a primary condition or a secondary condition to a different infection or disease. Genetic mutations and environmental factors are often factors, but at other times the cause of the disease remains unknown.
To mark World Amyloidosis Day, this article aims to demystify the condition, which not only affects the individuals who have it but also their caregivers and loved ones, as to foster a supportive environment for patients and their families.
Types of amyloidosis
To date, 36 different types of amyloidosis have been described. They’re characterized according to the type of protein found to be misfolded.
There are 19 proteins grouped as localized forms, 14 grouped as systemic forms, and three that can be either. All amyloid fibril proteins start with the letter "A," followed by the protein suffix and any applicable specification.
Some of the most common forms are described below.
Light-chain amyloidosis: AL amyloidosis affects the kidneys, spleen, heart and other organs, mainly in people with conditions such as multiple myeloma or a bone marrow illness called Wadenström’s macroglobulinemia. In AL, the plasma cells produce excess light chains that spread through the bloodstream and accumulate in tissue, damaging vital organs. AL amyloidosis is acquired, not inherited, and usually diagnosed in people over the age of 50.
Serum amyloid A amyloidosis: AA amyloidosis affects kidneys and liver, particularly in individuals with long-term inflammatory conditions, such as rheumatoid arthritis, or chronic infections, such as tuberculosis. In AA amyloidosis, a protein produced in the liver called serum amyloid A misfolds and forms amyloid fibrils, disrupting organ functions. People of any age are affected by AA amyloidosis, and it is the most common form of amyloidosis in children.
Amyloid transthyretin amyloidosis: ATTR amyloidosis affects the heart, peripheral nerves and the autonomic nervous system. It occurs when transthyretin (also known as prealbumin), a protein produced in the liver, misfolds. There are two types of ATTR amyloidosis: an acquired form known as wild-type ATTR amyloidosis (wtATTR amyloidosis) and a hereditary form called hereditary ATTR amyloidosis (hATTR amyloidosis), also known as familial amyloidosis. wtATTR typically occurs in people over 70 and is more common in men than in women. hATTR occurs largely in teens and young adults, depending on the mutation involved.
Localized amyloidosis: Localized amyloidosis is referred to as organ-specific amyloidosis, as it affects a single organ. It commonly affects the skin, bladder, eyes, respiratory system, or central nervous system. The most well-known type of localized amyloidosis is Alzheimer’s disease.
Many varied symptoms
Different types of amyloidosis affect varied organs and tissues, making the symptom list long and varied. The most common symptoms include purple spots (purpura) or bruised-looking areas of skin around the eyes, bleeding more than usual after an injury, increased tongue size, shortness of breath, feeling very weak or tired, weight loss, swelling in the abdomen and legs or feet, numbness, pain in hands or feet and skin that bruises easily.
Organ-specific symptoms are often described in amyloidosis. Affected kidneys produce foamy urine due to the presence of protein in urine and reduced urine output. Affected hearts have irregular heartbeats, causing shortness of breath during physical activity or while just lying down.
How it’s diagnosed
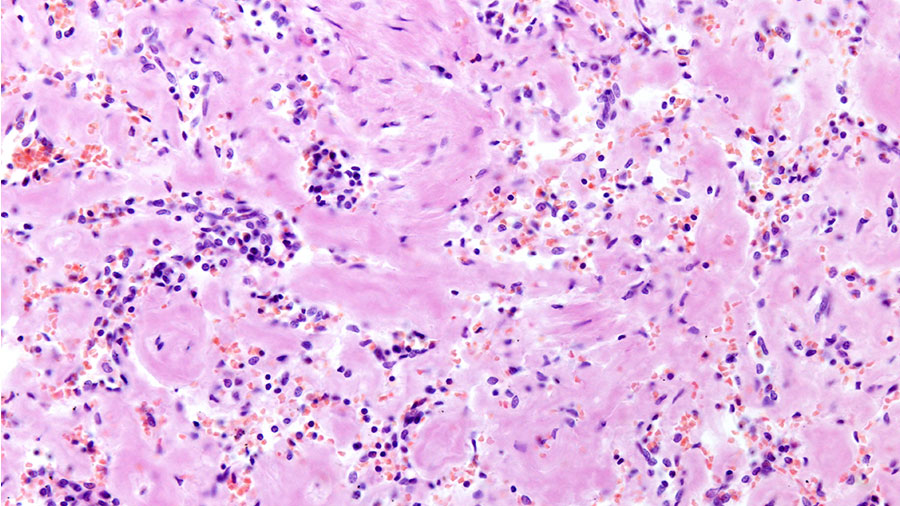
A physician will go over a patient’s medical history and conduct a physical exam, but diagnosis often requires tissue biopsy for the detection of amyloid deposits.
If deposits are found, additional testing — including genetic testing — is done to determine the specific protein involved.
Blood and/or urine analysis can assess organ function; imaging studies (such as ultrasound, MRI and X-ray) can determine which organs are affected; and organ-specific tests can measure functionality, such as an electrocardiogram for evaluating heart health.
How it’s treated
There is no cure for amyloidosis, but treatment can slow progression to improve patients’ quality of life.
Different forms demand varied treatments.
For patients with Al amyloidosis, chemotherapy stops the growth of cells producing abnormal proteins, and bone marrow transplants replace unhealthy cells destroyed by the chemotherapy.
Medications to stabilize proteins are given too. For example, tafamidis is used to treat ATTR amyloidosis as it stabilizes the transthyretin protein and prevents it from misfolding.
People with AA amyloidosis take drugs to reduce inflammation and clear infections, as AA amyloidosis occurs in patients with chronic inflammatory diseases and infections.
Medications to reduce the levels of abnormal proteins are also prescribed. For example, patisiran and inoteseren reduce the production of the transthyretin protein involved in ATTR amyloidosis.
Focusing on the facts
Amyloidosis remains a relatively enigmatic condition due to many misconceptions.
Prevalence: Although it is a rare disease, in recent times the number of reported cases has been steadily increasing due to better identification and diagnosis.
Affected population: Contrary to the general assumption that the geriatric population is predominantly affected, amyloidosis can affect individuals of any gender at any age.
Causes: Amyloidosis can be a primary or a secondary condition. There are different kinds of amyloidosis, and some of them are hereditary. Some forms strike people with infections or conditions that cause chronic inflammation.
Curability: Amyloidosis is not currently curable, but promising treatment options are available to significantly improve patients’ life quality.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

The data that did not fit
Brent Stockwell’s perseverance and work on the small molecule erastin led to the identification of ferroptosis, a regulated form of cell death with implications for cancer, neurodegeneration and infection.

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

