From the journals: JLR
What activates T cells in psoriasis? Lysosomal acid lipase in liver disease. A controlled diet targets heart disease risk. Read about papers on these topics recently published in the Journal of Lipid Research.
What activates T cells in psoriasis?
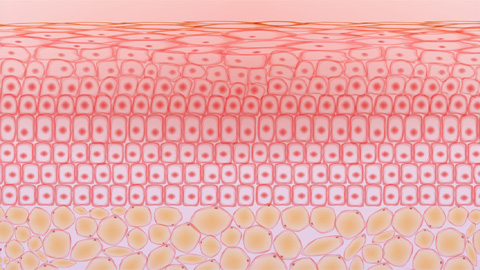
Psoriasis is a disease commonly identified by lesions; skin cells proliferate, white blood cells infiltrate and lipid metabolism is altered in the skin. In the past, researchers have shown that n-3 polyunsaturated fatty acids, or PUFAs, may suppress this inflammation, thus slowing disease progression. A recent study in the Journal of Lipid Research by Sophie Morin and a team at Laval University aimed to identify the role of n-3 PUFAs — specifically eicosapentaenoic acid, or EPA — in T cell activation and polarization in psoriasis.
Characteristically, psoriasis causes an increase in IL-17A, an inflammatory cytokine produced primarily by the Th17 subset of helper T cells, commonly known as CD4+ T cells. Morin’s team found that, in the presence of EPA, IL-17A production is reduced, and FOXP3+ regulatory T cell production increases. They determined that EPA inhibition of STAT3, a signaling protein on the cell surface that activates and polarizes Th17 cells, prevented polarization to a Th17 proinflammatory phenotype. This inhibition was specific to STAT3; EPA did not reduce polarization to a proinflammatory Th1 phenotype via STAT1.
The researchers used a 3D model of psoriatic skin to show that EPA reduced proliferation of skin cells, transduction protein phosphorylation and transcription activation. They also noted that the NF-κB pathway was altered, which led to increased concentrations of Fas, a death receptor located on the cell surface, causing increased cell death.
The researchers deduced that EPA and other n-3 PUFAs act as antiinflammatory mediators of psoriasis by simultaneously producing regulatory T cells and reducing proinflammatory T cell phenotypes, as well as altering major signaling pathways promoting psoriasis symptom reduction.
Lysosomal acid lipase in liver disease
Lysosomal acid lipase, LAL, plays a key role in metabolism and is the only enzyme known to degrade both cholesteryl esters and triglycerides at an acidic pH. Dysfunction of LAL causes a rare, autosomal recessive genetic disorder known as LAL deficiency, or LAL-D, and researchers have found that reduced LAL activity contributes to the progression of nonalcoholic fatty liver disease, or NAFLD. In a recent paper published in the Journal of Lipid Research, Ivan Bradić at the Medical University of Graz and collaborators aimed to learn more about liver-related pathologies of LAL through proteomic profiling.
In mice genetically altered to systemically lack the LAL gene, the researchers noted significant alterations in the proteome compared to their wild-type counterparts and to mice genetically altered to lack hepatocyte-specific LAL. Results indicated substantial liver remodeling, upregulation of glycolysis-associated proteins, increased cholesterol metabolism and hydrolase concentration, and decreased production of proteins associated with lipid and fatty acid metabolism.
Evidence of macrophage abundance, immunity, autophagy, apoptosis and immune processes involving myeloid cells increased in the mice lacking the LAL gene, suggesting higher levels of inflammation. This suggests metabolic alteration, inflammation and restructuring of the liver in LAL-D or NAFLD, which is most strongly modeled in models systematically lacking the LAL gene. These findings will aid in further characterization and potential therapeutic development for NAFLD.
Controlled diet targets heart disease risk
Saturated fatty acids, or SFAs, are found in foods such as full-fat dairy, red meat and poultry. Scientists have linked SFAs to production of low-density lipoprotein cholesterol, or LDL-C, which increases the risk of cardiovascular disease, or CVD. In the past, researchers have found that lipoprotein(a), or Lp(a), is similar to LDL-C, but poses an independent risk for CVD. While these factors are true for most ethnicities, individuals of African American descent experience a higher risk. For this reason, Hayley G. Law at the University of California, Davis and her collaborators aimed to identify an SFA-dependent relationship between Lp(a) and CVD risk in African American populations. They wrote about their work in a study recently published in the Journal of Lipid Research.
Study participants ate two diets sequentially, each for five weeks. The first was similar to the average American diet, or AAD, while the second contained a decreased amount of SFA. This diet resembles the dietary approaches to stop hypertension, or DASH, diet, which was supplemented with carbohydrates. As expected, switching from an AAD diet to a DASH diet resulted in a significant reduction in cholesterol, specifically LDL-C. Lp(a) levels were increased upon switching to the DASH diet, which the researchers speculate may be due to the carbohydrate supplementation. In the future, they may examine this relationship more deeply, determine the specific mechanisms that cause Lp(a) increases with SFA reduction and identify appropriate nutritional replacements.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Defining JNKs: Targets for drug discovery
Roger Davis will receive the Bert and Natalie Vallee Award in Biomedical Science at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

