Harnessing good fats to relieve MS symptoms
Basic nutrition teaches that fat, when consumed in large quantities, is harmful to human health. However, the components that make up fats are complex. Good, unsaturated fats, or lipids, can lower disease risk. In fact, in a new study, researchers found that a good fat derivative may be able to relieve symptoms in patients suffering from chronic inflammatory diseases, such as multiple sclerosis. They published their results in the Journal of Biological Chemistry on Jan. 7.
The study was conducted by Justin Kim, a postdoctoral fellow at the Georgia Institute of Technology, Aditi Das, an associate professor of chemistry and biochemistry at Georgia Tech, Andrew Steelman, an associate professor of animal sciences at the University of Illinois at Urbana-Champaign, and their colleagues.
MS is a chronic, autoimmune disease of the brain and spinal cord during which the immune system attacks the cells and tissues that protect nerve fibers. This potentially debilitating disease can cause pain, vision loss, fatigue, impaired cognitive function and more. There is no cure for MS, and it affects almost 1 million people nationwide.
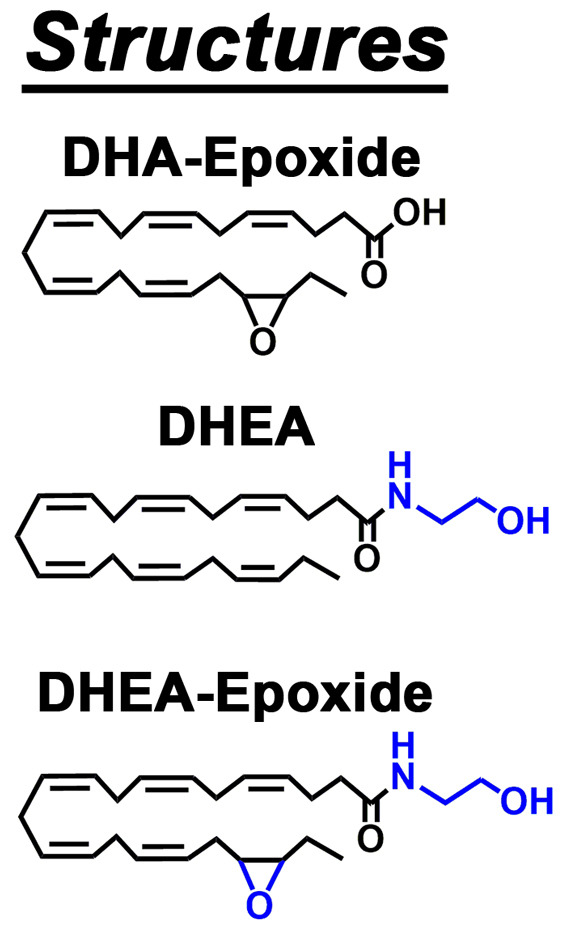
The researchers specifically looked at docosahexaenoyl ethanolamide (DHEA), a derivative of the lipids found in cold-water fish and fish oil supplements, and its impact on the immune system. Interestingly, DHEA has been shown to be anti-inflammatory and has similar properties to cannabis in some contexts.
“Our goal was to use something that is naturally found in food and the human body to see if we can enhance it to reduce the disease severity in multiple sclerosis patients,” Das said.
Using a common mouse model that closely mimics the relapsing and remitting nature of MS, Kim, Steelman and Das noticed that DHEA is at its highest concentration in the mice when they are in a state of remission, which prompted them to consider if DHEA could dampen the inflammation that controls the disease.
“We thought if we could somehow alleviate, control or reduce the level of inflammation, we could improve the disease outcomes and severity,” Kim explained.
Even though taking fish oil supplements has been linked to improved quality of life in patients with inflammatory conditions, the interworking of this association has never been teased apart in MS, until now. Kim, Steelman and Das were the first to show that the DHEA lipid can reduce inflammation and disease signs in a mouse model of MS. The researchers found that, when they supplemented the diet of mice with DHEA, the mice showed less severe and later onset of MS-like disease. This reduction is likely due to the presence of fewer activated, pathogenic T cells in the central nervous system, the research team found.
“We believe our findings could lead to the discovery of new solutions to aid in managing symptoms of multiple sclerosis and other chronic inflammatory diseases like diabetes,” Das said.
So, should you start taking fish oil supplements? First, more work is needed to study how DHEA affects other parts of the immune system and humans. However, the researchers are optimistic that this is a step forward in using naturally occurring good fats or their derivatives to lower inflammation without the negative side effects of some currently prescribed medications.
“I’ve seen that a lot of patients with multiple sclerosis are fully in tune with the research,” Kim said. “They are always trying to do everything that they can to improve their symptoms, whether it be through exercise, diet or just healthy living, while trying to reduce their consumption of heavy pain medications.”
The National Multiple Sclerosis Society advises patients reasonable doses of fish oil and omega-3 fatty acid supplements are generally safe and may be beneficial. However, patients should consult with their doctors before changing their medications, and supplements should never be used as a replacement for conventional therapies.
“There is no cure for MS, yet, and anything to help improve the patients’ symptoms is always of interest,” Kim said.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

