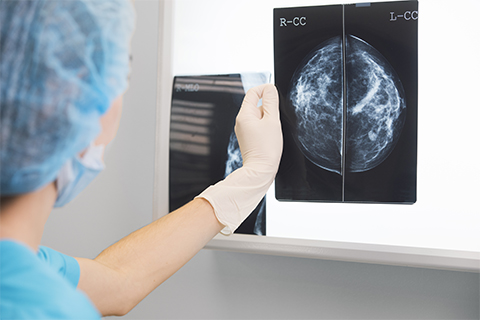
Study finds why immunotherapies don’t work on hardest-to-treat breast cancers
Thanks to advances in cancer therapies, most forms of breast cancer are highly treatable, especially when caught early.
But the last frontier cases — those that can’t be treated with hormone or targeted therapies and don’t respond to chemotherapy — remain the deadliest and hardest to treat. Tulane University researchers have discovered for the first time how these cancers persist after chemo and why they don’t respond well to immunotherapies designed to clear out remaining tumor cells by revving up the immune system.
The process of surviving chemotherapy triggers a program of immune checkpoints that shield breast cancer cells from different lines of attack by the immune system. It creates a “whack-a-mole” problem for immunotherapy drugs called checkpoint inhibitors that may kill tumor cells expressing one checkpoint but not others that have multiple checkpoints, according to a new study published in the journal Nature Cancer.
“Breast cancers don't respond well to immune checkpoint inhibitors, but it has never really been understood why,” said corresponding author James Jackson, associate professor of biochemistry and molecular biology at Tulane University School of Medicine. “We found that they avoid immune clearance by expressing a complex, redundant program of checkpoint genes and immune modulatory genes. The tumor completely changes after chemotherapy treatment into this thing that is essentially built to block the immune system.”
Researchers studied the process in mouse and human breast tumors and identified 16 immune checkpoint genes that encode proteins designed to inactivate cancer-killing T-cells.
“We’re among the first to actually study the tumor that survives post-chemotherapy, which is called the residual disease, to see what kind of immunotherapy targets are expressed,” said the study’s first author Ashkan Shahbandi, an M.D./Ph.D. student in Jackson's lab.
The tumors that respond the worst to chemotherapy enter a state of dormancy — called cellular senescence — instead of dying after treatment. Researchers found two major populations of senescent tumor cells, each expressing different immune checkpoints activated by specific signaling pathways. They showed the expression of immune evasion programs in tumor cells required both chemotherapy to induce a senescent state and signals from non-tumor cells.
They tested a combination of drugs aimed at these different immune checkpoints. While response could be improved, these strategies failed to fully eradicate the majority of tumors.
“Our findings reveal the challenge of eliminating residual disease populated by senescent cells that activate complex immune inhibitory programs,” Jackson said. “Breast cancer patients will need rational, personalized strategies that target the specific checkpoints induced by the chemotherapy treatment.”
This article first appeared in Tulane News. Read the original.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

