A new way of looking at concussions
On a crisp September day, Zoe Aldrich walked onto a rugby pitch on a college campus in upstate New York. With her teammates surrounding her, she got ready for the kickoff and the pitch became a blur of colored jerseys. A teammate passed Aldrich the ball and she started running, but an opposing player tackled her to the ground. Players collided above her, competing for the ball. As Aldrich tried to crawl out from under them, one of her teammates accidentally kicked her in the head. “I never lost consciousness,” she says, “but I didn’t feel well.”

Trainers diagnosed her with a concussion, and for the next year and a half, Aldrich suffered from a feeling of fogginess, like her brain wasn’t working correctly. People told her she would feel better in two weeks, then four, then six. Eventually, she says, “I had to give up on this notion that I had to wait a certain number of weeks and then things would go back to normal.”
Each year in the United States, there are around 3.8 million concussions, and sports- and recreation-related activities are responsible for a significant number of them. Most patients experience symptoms similar to Aldrich’s — headaches, nausea, fatigue, dizziness and memory loss. There is no single test to diagnose a concussion; instead, doctors examine balance, coordination, ability to pay attention, and memory. If the symptoms are severe, they’ll also conduct brain scans to check for swelling or bleeding.
For around 80 percent of patients, symptoms go away within two weeks. But others, like Aldrich, experience symptoms for months or even years. A history of multiple concussions may increase the risk of more serious problems later in life, including Alzheimer’s disease and chronic traumatic encephalopathy, or CTE, a neurodegenerative disorder with dementia-like symptoms.
Although it’s clear that concussions damage the brain, exactly how they do so is still largely a mystery — especially when it comes to long-term problems. An intriguing new clue focuses on tiny tubes sandwiched between the meninges, a set of membranes that surrounds and protects the brain and spinal cord. These tubes, called meningeal lymphatic vessels, help to clear cellular and molecular waste from the brain. A mouse study published in September in the journal Nature Communications reported that after minor blows to the head, the brain swells and pins these vessels up against the skull. Like putting a kink in a hose, this diminishes their ability to drain properly.
This damaged drainage system, the researchers speculate, may be what leads to more severe and longer-lasting symptoms.
“We know that most of the time, a concussion is a limited process; most people recover and don’t have long-term effects,” says Ann McKee, a neuropathologist who directs Boston University’s CTE Center and was not involved in the study. But in autopsies of people who had suffered from CTE during their life, McKee has found scarring in the meninges. “The idea that meningeal lymphatic channels may contribute to inflammation and persistent symptoms, I think, is a very interesting idea — it makes a lot of sense to me.”
The brain’s trash collection system
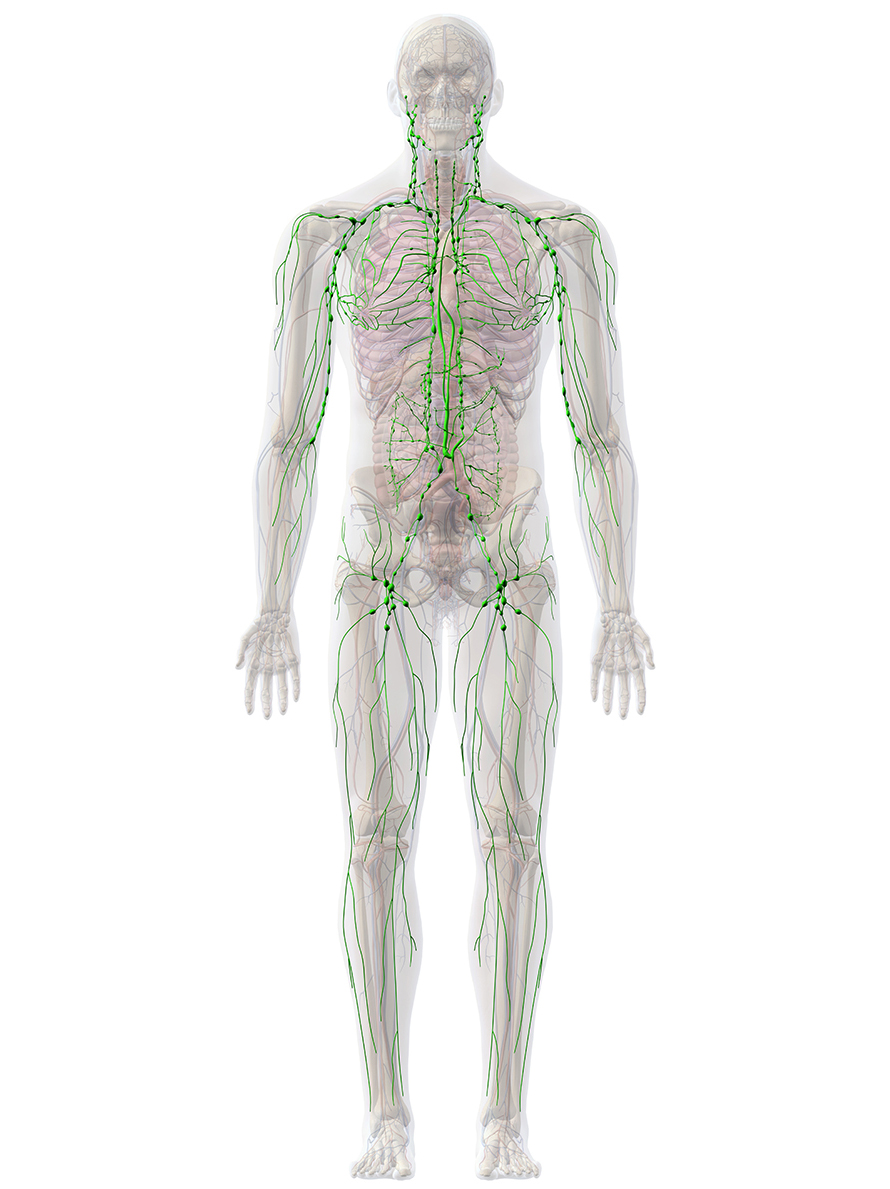
The existence of lymphatic vessels surrounding the brain was confirmed only recently — in 2015 — but scientists have long known that they exist elsewhere in the body, mingled among the veins and arteries that supply oxygen and nutrients to tissues and organs. This network of tiny, thin-walled tubes acts as the body’s molecular trash collection system. The vessels collect the clear fluid called lymph that leaks from the bloodstream — filled with immune cells as well as proteins and molecular debris. These are transported to lymph nodes, small structures throughout the body that filter out the harmful waste.
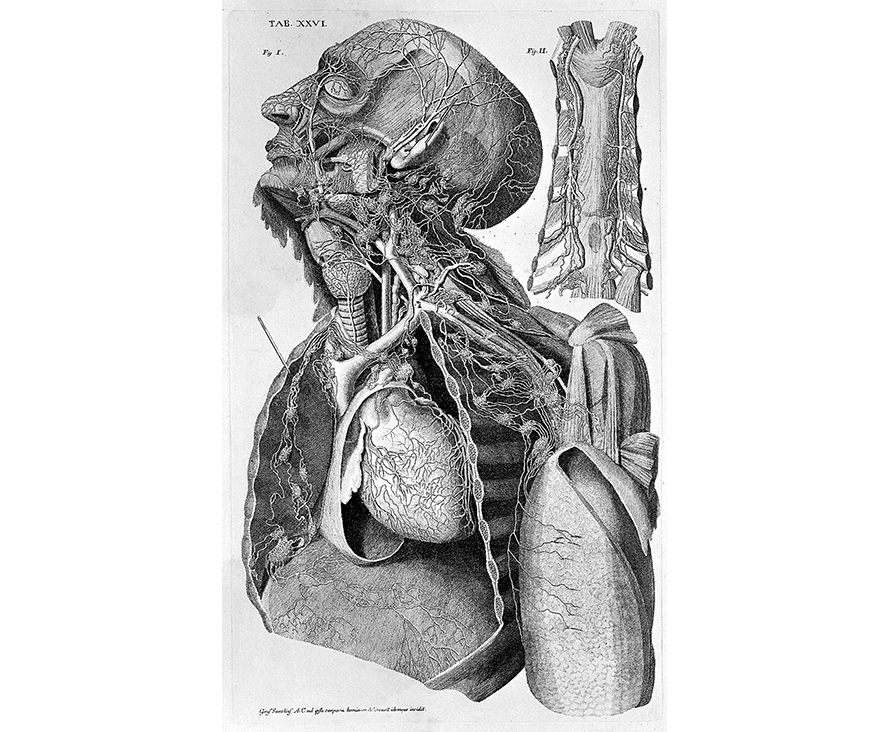
In the eighteenth century, Italian physician Paolo Mascagni created a detailed atlas of the lymphatic system and depicted these vessels in the meninges around the brain. But other scientists dismissed the idea, arguing that the lymphatic system was completely separate from the central nervous system. That remained the consensus for more than 200 years.
Then, in 1996, scientists looking at brain tissue with an electron microscope discovered structures in the meninges that looked like lymphatic vessels. Other researchers still weren’t convinced, writing off the tubes as capillaries, which are also thin-walled vessels. Finally, in 2015, neuroimmunologist Jonathan Kipnis, now at Washington University in St. Louis, and his former colleagues at the University of Virginia examined the brains of mice and uncovered a web of channels that resembled the lymphatic vessels found in the rest of the body.
To confirm that the tubes were not blood vessels, the scientists sacrificed the mice and removed their meninges, which they then stained with fluorescent molecules that bind to lymphatic cells, revealing meningeal lymphatic vessels. These vessels, which have since been found in other animals, including people and other primates, drain waste from the brain to a set of lymph nodes located next to the jugular vein in the neck.
Before this discovery, scientists weren’t sure how the brain disposed of waste after an injury. Following a significant hit to the head, brain cells die, releasing molecules that initiate inflammation and signal the immune system to clean up the damage. Inflammation immediately after an injury can help in the recovery process. But animal studies have shown that a flawed immune response can lead to chronic inflammation, which ultimately causes more cell death, damage to the ability of neurons to communicate, and other long-lasting neurological issues.
Kipnis thinks that the brain’s waste pathway might play a role in degenerative diseases like Alzheimer’s, where cell-damaging molecules called amyloid-beta accumulate between neurons and are not properly cleared. Over the past five years, he and his team have discovered that damage to the lymphatic vessels in mice increases the accumulation of amyloid-beta in mouse brains.
Kinks in the cleanup system
Down the hall from Kipnis’s former lab at the University of Virginia was another team of researchers who, inspired by his work, began investigating whether lymphatic vessels play a role in concussions. Graduate student Ashley Bolte and immunologist John Lukens worked with mice to see whether a blow to the head affected the rodents’ lymphatic vessels.
After giving the mice a mild blow with a device that dropped a small metal rod on their heads, Bolte monitored their alertness, balance and reflexes and found that their behavior didn’t change. She then injected tiny fluorescent beads into the cerebrospinal fluid to measure bead flow through the meninges, lymphatic vessels and lymph nodes. By looking at the meninges and lymph nodes under a microscope, Bolte discovered that the lymphatic vessels’ ability to drain was significantly diminished starting just two hours after the injury and lasting up to two months. This suggests that even blows to the head that aren’t hard enough to cause symptoms can damage lymphatic vessels.
Recent studies have also shown that the drainage ability of lymphatic vessels worsens as mice age. If that’s also true in humans, it might be one reason older people have longer recovery times and increased mortality rates from concussions. To simulate the effects of aging, Bolte destroyed part of the vessels in some mice by injecting them with a light-activated drug and shooting a laser through their skulls before giving them a mild hit to the head. Then she tested the rodents’ balance and coordination by putting them on a rod that began to rotate slowly and gradually accelerated over a span of five minutes.
Mice whose lymphatic vessels had been damaged had worse balance and motor coordination than mice with a concussion alone, she found. This suggests that preexisting lymphatic damage worsens the symptoms of concussion, she says.
Another set of experiments revealed that lymphatic damage also worsens memory impairments in mice after a hit to the head. In a standard test of rodent memory, Bolte put mice in a room with two plastic boxes for 10 minutes. She then removed the mice and moved one of the boxes. When she returned the animals 24 hours later, mice without damaged lymphatic vessels spent more time examining the box that had moved — an indication they knew something had changed. Mice with lymphatic damage didn’t do this, suggesting that they could not remember where the boxes had been the day before.
These findings by Bolte and Lukens, reported in their recent Nature Communications paper, may apply to athletes with a history of multiple concussions, who likely have damaged lymphatic vessels that don’t have time to repair in between hits, Lukens says. The study “shows that even mild hits to the head can cause long-lasting ‘kinks’ in the lymphatic pathway,” he says. “Maybe one reason why repetitive traumatic brain injuries are so detrimental is that you have these kinks beforehand from smaller hits.”
Bolte and Lukens also began wondering if it might be possible to reduce the long-term impacts of concussions by fixing the faulty pipes. They knew that past studies in adult mice had reported that a protein called vascular endothelial growth factor C, or VEGF-C, can increase the diameter of lymphatic tubes and therefore enhance their ability to drain. And so the researchers introduced VEGF-C into the meninges of some old and some young mice and gave them a mild blow to the head two weeks later.
Following the concussions, the brains of old mice that hadn’t received VEGF-C had dangerously high levels of macrophages and microglia, cells that respond to an injury by removing damaged cells and molecular debris and can cause damage if left unchecked. But the old mice receiving VEGF-C had many fewer of these cells in their brains. To the scientists, this finding suggests that by promoting growth in the lymphatic vessels, VEGF-C improves drainage and reduces inflammation in the brain, thus decreasing the injury’s intensity. “The growth factor fixes the faulty pipes that drain all of the bad things from our brain,” Lukens says.
This finding opens up the possibility that athletes could be treated with VEGF-C after a concussion to reduce brain inflammation and long-term complications, Lukens adds. But the findings are preliminary, and VEGF-C treatment is yet to be tested in people with a concussion.
The researchers also stress that lymphatic vessels aren’t the only part of the brain damaged after a concussion. Scientists have found that small hits to the head in mice impair the ability of neurons to take up dopamine, a key player in the brain’s memory process, which may be what leads to memory problems in concussion patients. Animal and human studies also have found that concussions injure axons, the long extensions on neurons that convey signals to neighboring neurons. This may cause a range of issues, including loss of consciousness and general confusion.
How exactly the lymphatic system is related to these other brain injuries is still unknown. “I think that injured lymphatic vessels are just one of many factors that are leading to the negative outcomes seen after traumatic brain injuries,” Bolte says.
A long road for athletes
If it panned out, a treatment like VEGF-C could be a game changer for athletes of all ages. Eric Nauman, a mechanical engineer at Purdue University, has been studying concussions for a decade. His research on high school football players has shown that repetitive hits to the head can lead to long-term issues, even if the patient isn’t showing symptoms initially. Lukens and Bolte’s study may explain one mechanism that makes these concussions so detrimental, says Nauman, who coauthored a recent paper reviewing the research on mild head injuries in the Annual Review of Biomedical Engineering.
Currently, there are no approved medications to treat concussions. Part of the reason is that the blood-brain barrier, which surrounds the brain and prevents most molecules from entering, is a great hurdle for drug delivery. But because the meninges are not guarded by the blood-brain barrier, it may be far easier to create a drug that reaches the lymphatic vessels, Kipnis says.
In the meantime, the best strategy is to prevent concussions from happening in the first place by, for instance, lowering the pressure of soccer balls or changing the stance of football players on the offensive line. “From my perspective, this is a totally solvable problem,” Nauman says.
Yet many athletes like Aldrich still risk getting a concussion when they walk out on the field. Six years after being diagnosed, most of Aldrich’s symptoms have resolved, but she still struggles at times to find and spell words. “I used to immediately catch spelling and grammar errors — they would never slip through before,” she says. “That part of me has changed.”
This article originally appeared in Knowable Magazine, an independent journalistic endeavor from Annual Reviews.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Defining JNKs: Targets for drug discovery
Roger Davis will receive the Bert and Natalie Vallee Award in Biomedical Science at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

