Spotlight on hematologic cancer
In recent years, cancer has emerged as a leading research topic due to its expansive effect on the body. The American Cancer Society estimates that this year about 1.9 million new cancer cases and 609,820 cancer deaths will be reported in the U.S. The National Cancer Institute predicts that this year there will be more than 80,000 new cases of non-Hodgkin lymphoma, almost 60,000 new cases of leukemia and more than 37,000 new cases of myeloma.
September is Leukemia and Lymphoma Awareness Month. This article will dive into the complexity and nuance of these conditions and cover recent and still-in-development therapeutic approaches.
What are leukemia and lyphoma?
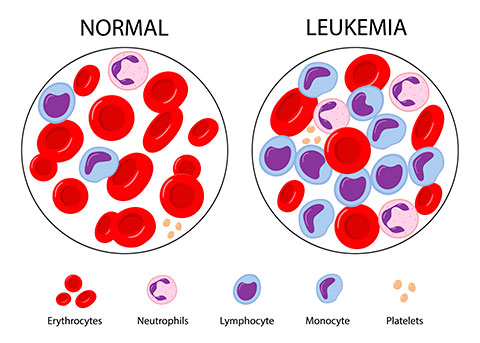
Leukemia is caused by the improper development and proliferation of leukocytes, which play a major role in the body’s immune system. During the maturation process, some leukocytes may begin to divide prematurely, producing a large quantity of dysfunctional cells. When this replication is allowed to continue it can cause malignancies, leading to cancer.
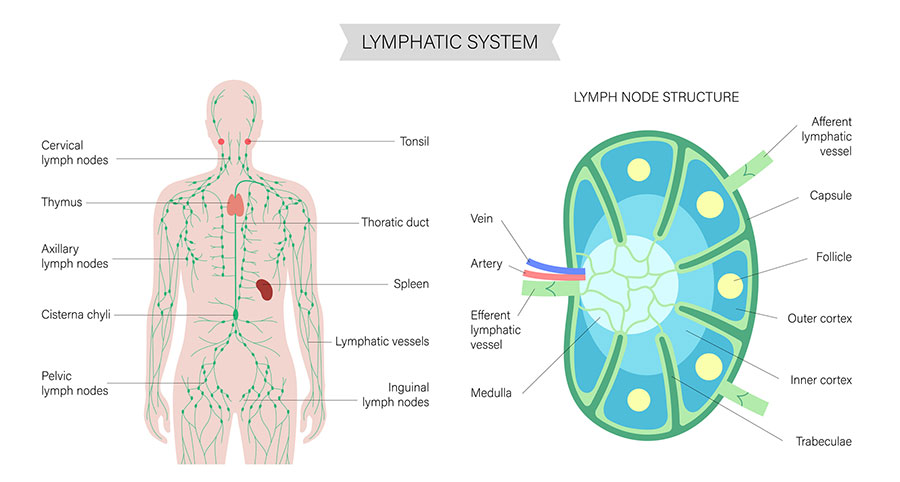
Lymphoma, conversely, is a cancer of the lymphatic system. Our body has a large quantity of lymph nodes, dispersed in areas such as our underarms, chest and neck. These nodes are responsible for production and release of immune cells, which fight infection throughout the body when released. White blood cells (a type of immune cell released by the lymphatic system) can sometimes develop genetic mutations, causing rapid proliferation.
A closer look at leukemia
Leukemia is often defined as either acute or chronic and myelocytic or lymphocytic, depending on the pace at which it progresses and the specific cells it impacts.
Acute leukemias consist of a higher concentration of blasts (also known as immature cells) in the blood, while chronic leukemia has a much lower blast concentration, which may not require immediate treatment.
Myelocytic leukemias affect myeloid stem cells, which are responsible for differentiation into red blood cells, platelets or granulocytes (a type of immune cell).
Lymphocytic leukemias affect lymphoid stem cells. These cells are responsible for differentiation into B cells, T cells and natural killer cells.
Four subtypes of leukemia account for a majority of diagnoses:
Acute lymphocytic leukemia: In acute lymphocytic leukemia, a disproportionately large quantity of stem cells become lymphoblasts, which then become B and T lymphocytes. These cells are consequently weakened in their immune response and are referred to as “leukemia cells.”
Research spotlight: Allogeneic stem cell transplantation
Stem cells are considered a viable method of treatment for leukemia and can be administered in conjunction with chemo or radiation therapy, both of which are known to weaken a patient’s immune system. By incapacitating the body’s natural defenses, donated stem cells are able to properly differentiate and stabilize a patient’s natural immunity.
Finding hematopoietic stem cell donors is quite the undertaking, according to the Leukemia and Lymphoma Society. It often requires identifying a donor with similar human leukocyte antigens to the patient. This prevents Graft-versus-host disease, in which donor cells begin to recognize healthy host cells as foreign bodies, ultimately destroying them and negatively impacting the patient.
When done correctly, donation of hematopoietic cells from donor to patient (a process known as “engraftment”) can significantly increase the amount of healthy immune cells in a leukemia patient.
As the number of leukemia cells in the blood increases, it becomes more difficult for normal, healthy cells to remain present and function properly in the blood, which causes a patient to present with symptoms such as fever, bruising, bleeding and infection, among others.
Treatment for ALL is broken down into different phases. The first phase of treatment is known as remission-induction therapy, in which the overall goal is to kill all leukemia cells and send a patient into remission.
From here, the second phase of treatment — known as post-remission therapy — is enacted. In post-remission therapy, the aim is to prevent future relapse of the condition by removing any remaining leukemia cells. Standard treatments used to combat ALL in one or both phases include options such as chemotherapy, radiation therapy, stem cell transplantation (often employed alongside chemotherapy) and targeted therapy using tools such as tyrosine kinase inhibitors or monoclonal antibodies. According to the American Cancer Society, clinical trials may also serve as a treatment option for some ALL patients.
Acute myeloid leukemia: Acute myeloid leukemia is an aggressive form and is most often observed in adult populations. According to the Leukemia & Lymphoma Society, AML may be caused genetically through mutation of bone marrow cells, genetic disorders such as Klinefelter syndrome or Down syndrome, or previous familial history of AML. Other factors include smoking, previous cancer treatment, age, sex and exposure to chemicals or radiation. There are different molecular subtypes, which can affect the prognosis of a patient.
Similar to ALL, AML presents with symptoms such as weakness, fever, infection, etc. Additionally, treatment strategies also include remission-induction and post-remission therapies. However, AML may require additional targeted therapies — such as protein kinase inhibitors and other drugs, such as arsenic trioxide and all-trans retinoic acid — in some patients.
Chronic lymphocytic leukemia: Chronic lymphocytic leukemia occurs when bone marrow produces an excess of lymphocytes. Symptoms often include swollen lymph nodes, weakness, fever, infection and petechiae, among others. CLL, unlike ALL or AML, is characterized in stages 0 through IV, depending on severity of the condition.
CLL is also classified as either asymptomatic, symptomatic/progressive, recurrent or refractory. Symptomatic/progressive CLL indicates a noticeable change in a patient’s blood count, while recurrent leukemia refers to CLL that returns after an undetectable period. Refractory leukemia is considered a type of CLL in which a patient’s condition does not improve with treatment.
Treatment for CLL includes methods such as chemotherapy, radiation therapy and stem cell transplant, all of which are often employed on other types of leukemia as well. However, CLL may also be treated with tactics such as immunotherapy (including approaches such as CAR T-cell therapy).
Chronic myeloid leukemia: Chronic myeloid leukemia is caused by a reciprocal translocation of genes on two nonhomologous chromosomes. BCR on chromosome 22 and ABL1 on chromosome 19 end up fused together to form the Philadelphia chromosome (abbreviated as Ph). Ph encodes for a tyrosine kinase protein and leads to overproduction of tyrosine kinase on chromosome 22. When this happens, a type of white blood cell known as granulocytes are unable to properly regulate, leading to overproduction and formation of cancer cells.
CML is often broken down into one of three phases — chronic, accelerated or blast — depending upon the amount of blast cells present in the blood and bone marrow.
Treatment for CML varies between each phase. Common treatment methods include targeted therapy using TKI, chemotherapy, immunotherapy, stem cell transplantation, lymphocyte infusion or surgery.
A closer look at lymphoma
There are many different subtypes of lymphoma, all of which have unique causes. The most common subtypes are Hodgkin and non-Hodgkin lymphoma.
Hodgkin lymphoma: As a cancer of the lymphatic system, Hodgkin lymphoma can originate in various parts of the body. It is most commonly seen near major sites of lymphoid tissue such as lymph nodes, bone marrow, the thymus and the digestive tract, among others. HL is classified as either classic or nodular lymphocyte-predominant HL
Classic HL: Classic HL is the most common type of HL and is caused by cancer cells known as Reed–Sternberg cells, which are often dysfunctional B lymphocytes. Classic HL is further categorized into four different subtypes.
- Nodular sclerosis HL: This is the most common type of classic HL. Typically, it originates in areas such as the neck and chest
- Mixed cellularity Hodgkin lymphoma: This is the second most common type of classic HL. MCHL is more common in those with an HIV infection and tends to recur in the upper half of the body.
- Lymphocyte-rich HL: This is an uncommon type of classic HL that is seen in the upper half of the body.
- Lymphocyte-depleted HL: This is a rare form of classic HL, which is often detected in older individuals and those who experience HIV infections. It is an aggressive form of cancer and is often identified once it is very advanced.
Nodular lymphocyte-predominant HL: NLPHL is a much less common form of HL, accounting for only about 5% of HL cases in the U.S.. It is caused by a Reed–Sternberg cell variant and often begins in the lymph nodes of the neck or under the arms. It is a slow-growing form of lymphoma.
Non-Hodgkin lymphoma: Non-Hodgkin lymphoma originates in lymphocytes and is treated differently than Hodgkin lymphoma. NHL affects either B-cells or T-cells and is categorized as either indolent or aggressive
B-cell NHL is the most common form of NHL, and it affects the body’s ability to produce antibodies and protect against foreign bacteria. T-cell NHL, conversely, affects cells that are responsible for destruction of germs and bolstering the body’s immune response.
Indolent NHL is considered slow in its growth and spread, similar to chronic leukemias. It often requires close monitoring but may not always require immediate treatment. Aggressive NHL, however, is quick in its spread and requires rapid response and treatment.
According to the American Cancer Society, the World Health Organization classification of NHL is dependent on factors such as the type of lymphocyte that the cancer originates in, physical appearance of the cancer cells, genetic features of the cells, and composition of the cell’s surface.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

