JLR: Technique boosts omega-3 fatty acid levels in brain 100-fold
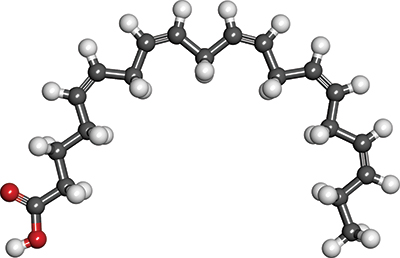 A ball-and-stick diagram of eicosapentaenoic acid, which has been shown to be effective in treating and preventing depression. SubDural12/Wikimedia Commons
A ball-and-stick diagram of eicosapentaenoic acid, which has been shown to be effective in treating and preventing depression. SubDural12/Wikimedia Commons
Getting enough docosahexaenoic and eicosapentaenoic acid, or DHA and EPA, into the brain to study their effects on conditions such as Alzheimer’s and depression — which they have been shown to help — is no easy task. While supplements containing these omega-3 fatty acids exist, there is scant evidence showing that the supplements actually increase DHA or EPA in the brain. To increase levels of EPA in the brain measurably, a person would have to consume a small glass of it each day, quite possibly with the side effect of smelling like fish.
Now researchers from the University of Illinois at Chicago report that adding a lysophospholipid form of EPA, called LPC-EPA, to the diet can increase levels of EPA in the brain 100-fold in mice. The amount of LPC-EPA in the diet required for this increase is rather small for mice — less than a milligram per day. The human equivalent would amount to less than a quarter of a gram per day.
DHA and EPA are known to have anti-inflammatory effects and protect against various neurological and metabolic diseases. DHA has been shown to be good for memory and cognitive deficits associated with Alzheimer’s disease, and, in studies, EPA has been shown to be effective in treating and preventing depression.
DHA is already prevalent in the brain, and there is little evidence to support the idea that eating lots of fish oil, either through whole fish or supplements, increases levels of DHA in the brain. EPA is found in very low concentrations in the brain, and boosting those levels through consuming EPA has proved difficult, because the amount that would need to be ingested to show increases in brain EPA levels is quite large — 40 to 50 milliliters daily. And researchers still don’t really have a great understanding of how EPA works to reduce depression and how much is needed in the brain to have these anti-depressive effects.
Papasani Subbaiah is a professor of medicine and biochemistry and molecular genetics in the UIC College of Medicine and corresponding author of a paper about the new work published in the Journal of Lipid Research.
“In order to do the trials to determine the proper dosage and how EPA works in regards to depression, we need to have a better way of getting it into the brain because you need to consume so much of it that it’s just not practical, at least for human trials,” Subbaiah said.
EPA provided in the form of lysophospholipid escapes the degradation by pancreatic enzymes that prevents the type of EPA in fish oil supplements from passing into the brain, he said.
“It seems that there is a transporter at the blood–brain barrier that EPA must pass through in order to get into the brain, but EPA in fish oil can’t get through, whereas LPC-EPA can,” Subbaiah said. “You don’t have to consume all that much LPC-EPA to have significant increases of EPA show up in the brain, so this could be a way to do rigorous studies on the effects of EPA in humans.”
Producing LPC-EPA is not difficult, and it can be incorporated into feed pellets that Subbaiah fed to laboratory mice. After eating 1 mg per day of the LPC-EPA in their feed for 15 days, these mice had up to 100 times more EPA in their brains than mice eating plain EPA. Interestingly, the mice eating LPC-EPA also had two times more DHA in their brains.
“This study is proof of the concept that we can increase levels of both EPA and DHA in the brain via supplements or by incorporating LPC-EPA in the diet,” Subbaiah. “Using this technique, we can now perform critical studies to see if increasing concentrations of these fatty acids in the brain can help prevent and treat Alzheimer’s and depression in mouse models, and then move into human trials if results are promising.”
This article is adapted from a press release produced by the University of Illinois at Chicago News Bureau.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.
