Is cholesterol a link between kidney and heart disease?
Each of the 11 major organ systems in the human body has a unique function that cooperates with the next to mediate homeostasis. These systems work together efficiently when a person is healthy; just think of how lightning-fast neural signals deliver cues from the brain to the muscles so you can move your hand off a hot stove. But, how do your systems affect one another in disease states? This is a question that researchers have begun to explore.
For example, researchers reported in 2004 that patients with chronic kidney disease, or CKD, were at an increased risk for cardiovascular disease, or CVD, with CVD being the leading cause of mortality in CKD patients. The kidneys filter waste from the blood, which is excreted as urine, and CKD is characterized by progressive loss of kidney function. The cardiovascular system pumps oxygenated blood to the organs and can be perturbed by diet, stress and other diseases, including CKD. But why would a patient with CKD be at an increased risk for CVD? How are these two systems related?
For more than 40 years now, researchers have demonstrated that low levels of high-density lipoprotein, or HDL —which carries low-density lipoprotein, or LDL, out of the arteries— is a risk factor for coronary heart disease, a type of CVD, in the general population. However, scientists know little about the mechanistic role of HDL cholesterol in CVD onset in CKD patients.
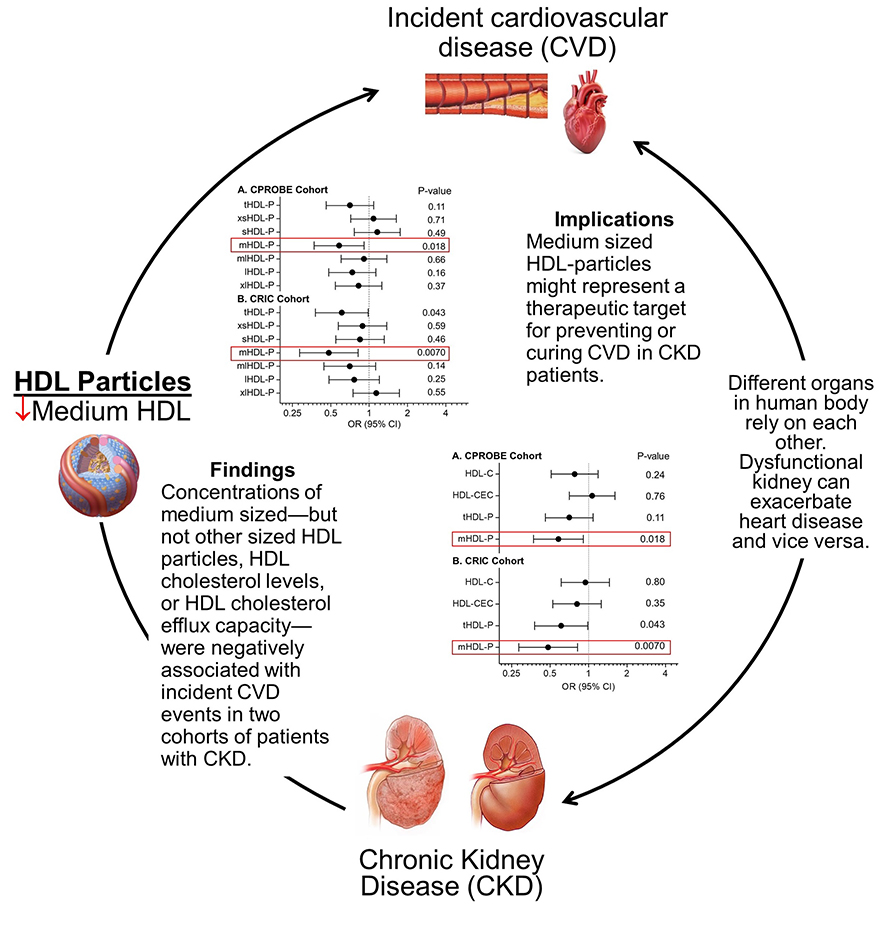
Baohai Shao from the University of Washington, Subramaniam Pennathur from the University of Michigan, and a team of researchers recently published a study in the Journal of Lipid Research investigating several HDL metrics, to determine how this lipid correlates with CVD risk in CKD patients.
The researchers examined two cohorts of CKD patients: 92 from the Clinical Phenotyping and Resource Biobank Core, 46 with incident CVD and 46 without, and 91 from the Chronic Renal Insufficiency Cohort, 34 with incident CVD and 57 without. In the baseline samples from these patients, they compared levels of HDL cholesterol, cholesterol efflux capacity and concentrations of HDL particles of sizes ranging from extra-small to extra-large. In both cohorts, levels of most of these metrics were not different in CKD patients with or without incident CVD; however, levels of medium-sized HDL — but not other sizes — were lower in CKD patients with incident CVD. This indicates that medium-sized HDL particles might have a cardioprotective function.
Different-sized HDL particles contain different combinations of proteins, the team noted, and medium-sized particles may house proteins with more protective functions, such as PON1, an enzyme that they previously showed was associated with incident CVD in CKD subjects when at low levels.
According to Shao, their current study “demonstrated that reduced levels of medium HDL particles, but not other sized HDL particles, can predict future CVD events in CKD patients. In addition to being an accurate marker to predict future CVD events, it raises the possibility that therapies that augment levels of medium HDL particles might be important to prevent CVD in CKD subjects.”
Overall, Shao’s group investigated why CKD patients are at increased risk for CVD, given the severity of both diseases. “If kidney disease worsens, waste can build up to high levels in your blood and make you feel sick, and it may eventually lead to kidney failure,” Shao wrote in an email. Moreover, “heart disease is the primary cause of death for all people with CKD.” This investigation into the relationship between the kidneys and the heart may improve efforts to treat and prevent CVD in CKD patients. “Medium-sized HDL can be an attractive marker,” Shao wrote, “that can be clinically useful to predict future events as well as potentially serving as a therapeutic target.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

