Raw milk is risky, but airborne transmission of H5N1 from cow’s milk is inefficient in mammals
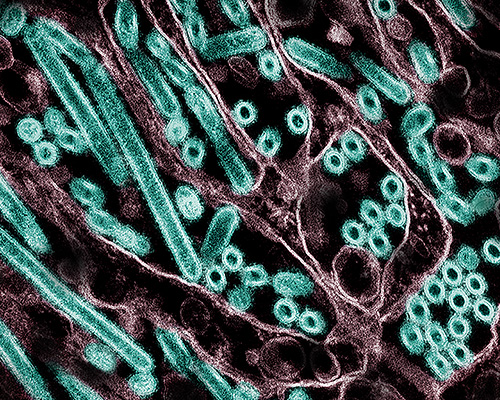
While H5N1 avian influenza virus taken from infected cow’s milk makes mice and ferrets sick when dripped into their noses, airborne transmission of the virus between ferrets — a common model for human transmission — appears to be limited.
These and other new findings about the strain of H5N1 circulating among North American dairy cattle this year come from a set of laboratory experiments led by University of Wisconsin–Madison researchers, reported today in the journal Nature. Together, they suggest that exposure to raw milk infected with the currently circulating virus poses a real risk of infecting humans, but that the virus may not spread very far or quickly to others.
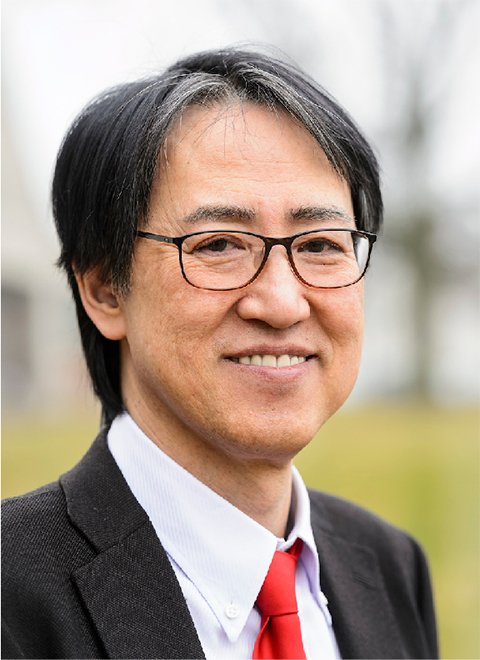
“This relatively low risk is good news, since it means the virus is unlikely to easily infect others who aren’t exposed to raw infected milk,” says Yoshihiro Kawaoka, a UW–Madison professor of pathobiological sciences who led the study alongside Keith Poulsen, director of the Wisconsin Veterinary Diagnostic Laboratory, and with collaborators at Texas A&M University, Japan’s University of Shizuoka and elsewhere.
Kawaoka cautioned, however, that the findings represent the behavior of the virus in mice and ferrets and may not account for the infection and evolution process in humans.
In their experiments, the UW–Madison team found that mice can become ill with influenza after drinking even relatively small quantities of raw milk taken from an infected cow in New Mexico.
Kawaoka and his colleagues also tested the bovine H5N1 virus’s ability to spread through the air by placing ferrets infected with the virus near but out of physical contact with uninfected ferrets. Ferrets are a common model for understanding how influenza viruses might spread among humans because the small mammals exhibit respiratory symptoms similar to humans who are sick with the flu, including congestion, sneezing and fever. Efficient airborne transmission would signal a serious escalation in the virus’s potential to spark a human pandemic.
None of the four exposed ferrets became ill, and no virus was recovered from them throughout the course of the study. However upon further testing, the researchers found that one exposed ferret had produced antibodies to the H5N1 virus.
“That suggests that the exposed ferret was infected, indicating some level of airborne transmissibility but not a substantial level,” Kawaoka says.
Separately, the team mixed the bovine H5N1 virus with receptors — molecules the virus binds to in order to enter cells — that are typically recognized by avian or human influenza viruses. They found that bovine H5N1 bound to both types of molecules, representing one more line of evidence of its adaptability to human hosts.
While that adaptability has so far resulted in a limited number of human H5N1 cases, previous influenza viruses that caused human pandemics in 1957 and 1968 did so after developing the ability to bind to receptors bound by human influenza viruses.
Finally, the UW–Madison team found that the virus spread to the mammary glands and muscles of mice infected with H5N1 virus and that the virus spread from mothers to their pups, likely via infected milk. These findings underscore the potential risks of consuming unpasteurized milk and possibly undercooked beef derived from infected cattle if the virus spreads widely among beef cattle, according to Kawaoka.
“The H5N1 virus currently circulating in cattle has limited capacity to transmit in mammals,” he says. “But we need to monitor and contain this virus to prevent its evolution to one that transmits well in humans.”
This article was republished from the University of Wisconsin-Madison News. Read the original here.Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

The data that did not fit
Brent Stockwell’s perseverance and work on the small molecule erastin led to the identification of ferroptosis, a regulated form of cell death with implications for cancer, neurodegeneration and infection.

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

