CRISPR nanoparticles are the next big hope in Alzheimer’s disease treatments
It’s hard to ignore the fanfare. CRISPR and other genome-editing technologies are set to redefine the way we treat a vast array of illnesses, from cancer to inherited genetic conditions. Hailed as the biggest biotech discovery of the century, CRISPR is enabling an exciting prospect: the ability to cure disease by directly and permanently modifying the human genome.
Naturally, there is a new wave of optimism that this technology can be leveraged towards a potential therapeutic for Alzheimer’s disease. Fueling this notion is CRISPR’s tangible impact on accelerating breakthroughs in Alzheimer’s research in the last five years. With access to this relatively cheap and easy to use technique, neuroscientists are now able to quickly identify new molecular pathways and design more elegant animal models to study neurodegenerative disorders.
Still, experts say that gene modification technologies alone are unlikely to translate into a solution for Alzheimer’s patients anytime soon, given the field’s bleak history of disappointment. A whopping 99.6% failure rate for new Alzheimer’s drugs, hundreds of failed clinical trials, billions of investment dollars lost. There are more questions than answers. Consequently, almost 6 million Americans live with Alzheimer’s – all without solid diagnostic, preventative, or treatment options.
Creating a CRISPR approach to treating diseases of the central nervous systems in humans poses several unique challenges. For one, the brain’s anatomical location and highly sensitive nature make drug administration tricky (and risky) business. Neuroscientists are faced with a conundrum: how to safely inject CRISPR into patients, shuttle it across the notorious blood-brain barrier, and target specific neurons, deep within the cerebrum?
On top of this, a far more fundamental dilemma exists - getting CRISPR into cells on a molecular level.
In order to make tweaks to faulty genes, CRISPR’s machinery (short RNA strands coupled with bulky Cas9 enzyme molecules) needs to cross the cell’s membrane, traverse the intricate intracellular space, dodge organelles, and eventually wind up inside the nucleus, where the genome is, to work its magic.
To do this, therapeutic developers have tried everything from zapping cells with electricity to using disarmed viruses to haul in the gene-editing cargo, all with mixed results and, unsurprisingly, considerable safety concerns. Erring on the side of caution, the FDA has approved only one CRISPR therapeutic to date. This cancer treatment, for which U.S. clinical trials started in May, uses an inactivated HIV strain to deliver CRISPR to the patient’s immune cell.
In March, a team of Korean researchers announced they have developed the nanoparticle equivalent of delivery drones for transporting CRISPR to brains with Alzheimer’s. Their findings were published in the journal Nature Neuroscience.
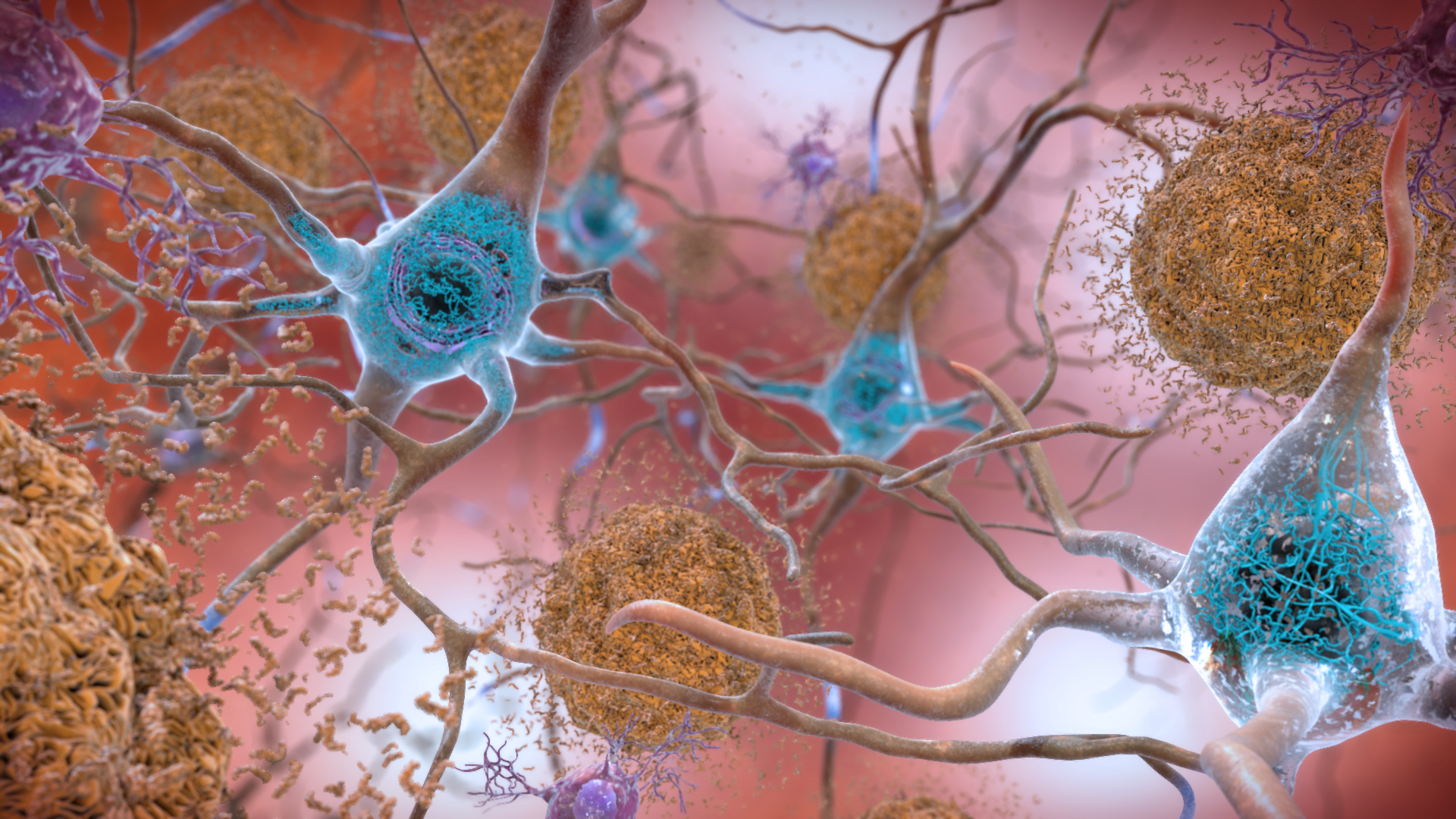
Biomedical engineer Jongpil Kim and his team created “nanocomplexes” for neurons - molecular bubble wrap used to encapsulate CRISPR components to specifically turn off the Bace1 gene. Bace1 is a prime therapeutic target, as it is known to stimulate amyloid beta (Aβ) production, which in turn has been linked to Alzheimer’s devastating cognitive effects.
Injecting these nanocomplexes into mice (genetically-modified to mimic the biological characteristics of the disease) was found to have remarkable effects. Not only did Bace1 and Aβ levels plummet in Alzheimer’s mice following a single dose, but memory and learning also dramatically improved compared to their untreated counterparts.
“It took a long time to collect the results from the Alzheimer’s mouse models,” says Kim, with longitudinal studies spanning a period of over three months, “but the most exciting moment was seeing the consistent and effective results.”
Still, with much of the genetic landscape around Alzheimer’s development being uncharted territory, an effective CRISPR delivery system alone will not be enough.
“Our scientific understanding of the brain and its disorders is not as advanced as other physiological systems,” says Troy Rohn, biology professor specializing in Alzheimer’s research at Boise State University. “Designing therapeutics where the molecular targets are not well defined is an obvious hurdle that we have yet to overcome.”
Several other technical wrinkles also need to be smoothed out if CRISPR is to live up to its hype. Of these, specificity and accuracy of the system remain major concerns. What are the chances of it making an error while editing a tiny fragment of our 3-billion-letter genome? Also, what are the consequences of those errors, especially considering all changes are permanent?
Speaking to the possibility of a CRISPR nanocomplex gene therapy in the near future, Kim says, “We need to test potential off-target effects extensively in the brains of higher primates first before we can translate our research to the clinic.” New computer software developed for predicting CRISPR’s precision in cells can also aid in endeavors to ensure safety prior to human trials.
Realistically, the odds of an Alzheimer’s cure being forged out of innovations in genetic technology, sadly, remain exceedingly slim. Still, CRISPR’s tremendous contributions to Alzheimer’s research drive progress and continue to inspire even a little bit of hope.
As Rohn optimistically reflects, “I believe this technique has the potential to be the most important tool in medicine for the next 50 years.”
This story originally appeared on Massive Science, an editorial partner site that publishes science stories by scientists. Subscribe to their newsletter to get even more science sent straight to you.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

