Researchers unmask
a pancreatic cancer culprit
Over the past decade, oncologists have made great strides in using immunotherapy to treat solid cancerous tumors that were unresponsive to other therapeutic approaches. One approach has been the development of checkpoint blockade therapy, which uses neutralizing antibodies to target two immune-response inhibitory proteins, CTLA-4 and PD-1, that are localized on the outer surface of cytotoxic T immune cells. However, pancreatic cancer has not responded to this immune-based treatment.
While the complexity and diversity of the tumor microenvironment — which contains myeloid cells, tumor-associated macrophages and regulatory B cells — might contribute to the repression of cytotoxic T cells and cause immunotherapy to fail, another factor in immune evasion might be biochemical or molecular changes in pancreatic cancer cells.
A significant immune response is induced when T cells engage with antigens presented on the outer surface of a cancer cell that are bound to a major histocompatibility complex class I, or MHC class I, molecule.
A growing number of researchers have proposed that the lack, or failure, of MHC molecules to present tumor antigens may be to blame for immune evasion of cancer cells. These MHC molecules include a beta 2-microglobulin protein encoded by the B2M gene and a protein encoded by human leukocyte antigen, or HLA, genes. These molecules help different antigens become engaged with different MHCs by exhibiting variation in the MHC motifs that bind to antigens.
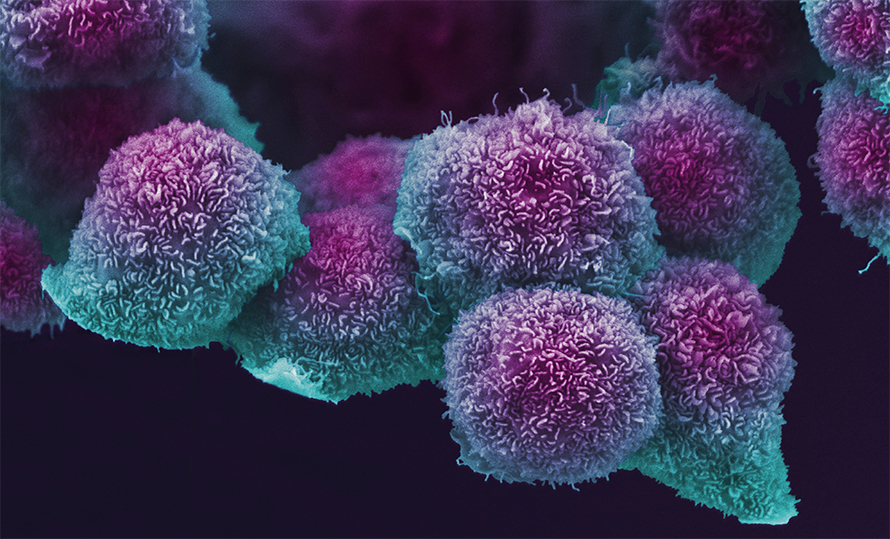
Although the failure to present cancer antigens — and the resultant immune evasion of pancreatic cancer cells — can occur at the transcriptional level through alterations in the genes that encode proteins required for antigen presentation, such as B2M and HLA, these genetic variations are rare in pancreatic cancer, accounting for less than 1% of total cases reported. Nevertheless, attenuated abundance or complete depletion of MHC class I molecules occurs in the majority of pancreatic cancer cells, and this reduction in MHC levels may be exacerbated in metastatic tumors.
The mechanisms underlying the regulation of MHC class I molecules in pancreatic cancer have remained elusive. Recent work published in the journal Natureshowed that autophagy, the cellular degradation machinery found across eukaryotes, is the mechanism pancreatic cancer cells use to break down MHC class I molecules, halting antigen presentation at the cell surface.
In their paper, researchers at New York University’s Perlmutter Cancer Center demonstrated that an autophagy-associated receptor, NBR1, mediates the engagement and subsequent targeting of MHC class I molecules by the autophagic degradation pathway. They also found that mitigating autophagy in mouse models of pancreatic cancer restored the expression of MHC class I molecules, which facilitated antigen presentation on cellular surfaces and enhanced recruitment of cytotoxic T cells to the tumor.
These insights might have direct therapeutic implications in pancreatic cancer, such as co-administration of the immunosuppressants chloroquine or hydroxychloroquine with the neutralizing antibodies.
RELATED ARTICLES
The odyssey of autophagy
In 2016, the Nobel Prize in physiology or medicine was awarded to Yoshinori Ohsumi for uncovering the mechanisms behind autophagy.
A legacy of tyrosine
Tony Hunter, a biochemist and former director of the Salk Institute Cancer Center, has begun to focus his research on pancreatic cancer and histidine kinases.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

