The other malaria parasite
The year 2010 saw 216 million cases of malaria and an estimated 655,000 deaths from the disease, according to the World Health Organization’s 2011 World Malaria Report. Ninety-one percent of the deaths occurred in tropical regions of Africa, and an overwhelming 86 percent of the dead were children under 5 years old. The most likely culprit of those cases was the parasite Plasmodium falciparum. Given its lethality, much research has been done over the past 40 years to try to wipe out the pathogen.
But P. falciparum is not the only parasite that causes deadly malaria: Plasmodium vivax is another that puts about 3 billion people living in other parts of the world at risk of contracting malaria. But because of the intense focus on P. falciparum’s ravages in Africa, malaria researchers say efforts to understand P. vivax malaria have been sorely neglected.
Malaria researchers say that the ignorance has to be rectified. P. vivax is rampant in Asia, South America and the southern Pacific. Ivo Mueller at the Walter and Eliza Hall Institute of Medical Research in Australia rattles off a few numbers to make the point: In Brazil, P. vivax accounts for 90 percent of malaria cases. In China, P. vivax causes between 80 and 90 percent of malaria cases. “There is no way, if you do malaria research outside of Africa, for you to ignore that parasite,” Mueller says.
But working with P. vivax is much more challenging than working with P. falciparum. Lee Hall, chief of parasitology and international programs at the National Institute of Allergy and Infectious Diseases, says the obstacles to studying P. vivax became grimly apparent when the Bill and Melinda Gates Foundation’s call to arms in 2007 for malaria eradication got researchers thinking deeply about how to achieve the goal. “There are a lot of scientific and technical hurdles that are still significant impediments. The clinical aspects too are quite challenging,” he says. If malaria eradication is to be achieved, says Hall, the scientific, technical and clinical issues surrounding P. vivax have to be understood. And therein lies the problem.
Neglect of a parasite
Malaria is a disease defined by chills, sweating and fevers brought on by the bursting of red blood cells and the possible release of toxins produced by Plasmodia parasites. Five parasites have been identified so far to cause malaria in humans: P. falciparum, P. vivax, P. malariae, P. ovale and P. knowlesi. The parasites are transmitted from person to person by the Anopheles genus of mosquito.
Current distribution analyses of pathogenic Plasmodium species in humans shows that P. falciparum is more prevalent in tropical regions, while P. vivax is more prevalent in South America. Both parasites are prevalent in southeastern Asia and the western Pacific.
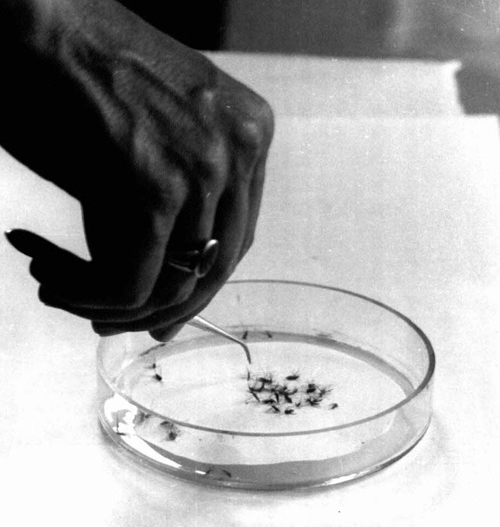 A mosquito-eradication campaign in Iran showed that mosquitoes eventually developed resistance against insecticides. This image was taken in 1958 in Iran when a World Health Organization team went to help the Institute of Parasitology and Malariology in Tehran organize field tests in the city of Shiraz, where mosquitoes were reported to be resistant. Philip Boucas/World Health Organization
A mosquito-eradication campaign in Iran showed that mosquitoes eventually developed resistance against insecticides. This image was taken in 1958 in Iran when a World Health Organization team went to help the Institute of Parasitology and Malariology in Tehran organize field tests in the city of Shiraz, where mosquitoes were reported to be resistant. Philip Boucas/World Health Organization
P. malariae can occur in all areas stricken with malaria, but its appearance is usually low. P. ovale is widespread mostly in tropical Africa, whereas P. knowlesi infection so far is known to occur only in certain forested areas of southeast Asia, such as in Malaysia.
Throughout the 20th century, P. falciparum infections were known as “malignant” malaria. In contrast, P. vivax infections got slapped with the unfortunate adjective “benign.” The word gave the impression that P. vivax didn’t send its victims to the grave. But that is not true. “The fatality rate with falciparum tends to be higher, but it doesn’t mean that vivax malaria is a benign disease,” says Mueller. “Vivax kills as well, just not as often.”
The notion that P. vivax wasn’t as dangerous as P. falciparum twisted its clinical record. There is speculation among malaria researchers that, as a result of colonial rule and medical standards of the day, medical doctors in India and other regions in the 19th and 20th centuries were not allowed to attribute the cause of death to P. vivax malaria, says Rhoel Dinglasan at the Johns Hopkins School of Public Health. They had to list a different infection simply because the conventional wisdom was that a P. vivax infection could not be lethal.
P. vivax’s neglect is also compounded by the fact that it is a trickier organism to study than P. falciparum. It has, thus far, eluded all efforts to be cultured stably in vitro. “We’ve been able to culture Plasmodium falciparum since the mid- to late 1970s. Because we can culture it, we have a huge arsenal of molecular and other tools,” says Mueller. The availability of P. falciparum in in vitro cultures means researchers can isolate large amounts of the parasite at close to 100 percent purity.
The lack of in vitro systems for P. vivax forces malarial researchers to purify the parasite from blood samples taken from patients. To confound matters, P. vivax infects only reticulocytes, which are young red blood cells that make up about 1 percent to 2 percent of a person’s total blood cell count. So the amount of parasite circulating through an infected person’s system is very low. The best researchers can do is to get about 80 percent purity with their preparations.
The lack of culturing methods also means that drug development against P. vivax is hard, says Mueller. For P. falciparum, in vitro assays allow researchers to screen libraries of potential drugs against the possible targets in the parasite. P. vivax lacks those in vitro assays, so drug screening is hard to do.
In short, malarial researchers studying P. vivax are in a tough spot. “Progress in vivax research is slower than in falciparum research,” says Mueller. “It takes more effort and more money to get the same kind of results as you would get for falciparum.”
Drugs and vaccines
In the current effort to eradicate malaria (there were other malaria eradication campaigns in the 20th century that failed), the Gates Foundation and other agencies have devoted resources in the past five years to develop new drugs to treat malaria cases and vaccines to halt the transmission of the parasites. For drugs and vaccines against P. vivax, the challenges are several-fold. One is P. vivax’s biology.
The parasite has several stages in its lifecycle that happen in different places in the mosquito and human bodies. The human blood circulation system is one such location. To date, clinicians have been able to treat P. vivax’s blood stages with common malarial drugs, because the parasite has not yet acquired the same kind of resistance P. falciparum has. But it may not remain so easy. “We can still treat vivax in many parts of the world with chloroquine, although choroquine resistance in vivax is rising,” notes Mueller.
 In the microscopy laboratory at Cambodia’s National Center for Malaria, personnel look at blood slides for malaria. World Health Organization.
In the microscopy laboratory at Cambodia’s National Center for Malaria, personnel look at blood slides for malaria. World Health Organization.
Unlike P. falciparum, which lives out the human part of its lifecycle in the blood, P. vivax has a dormant stage while it is in the human liver. Even if the blood-circulating form of P. vivax gets cleared out by drugs, the parasite can continue to lurk hidden deep inside the liver, and the person carrying the dormant P. vivax doesn’t show any symptoms of malaria. Then, by an unknown mechanism, the parasite bursts forth anywhere between a few months to several years after initial infection, infects the reticulocytes and causes the patient to relapse with malaria. Mosquitoes pick up the parasites from infected people and spread them, continuing the cycle of transmission.
Mario Henry Rodriguez-Lopez at the National Institute of Public Health in Mexico says this dormant form of P. vivax is a major problem. He describes how patients get treated with chloroquine for the blood forms but 10 percent of those patients end up relapsing, because the dormant P. vivax emerges from the liver and sets off another cycle of infection. In contrast, P. falciparum doesn’t have a dormant stage, so it always can be targeted in the blood with drugs, assuming it hasn’t acquired resistance to those drugs.
A drug called primaquine attacks P. vivax when it’s in the liver, but the drug has some serious drawbacks. Primaquine can’t be administered to children and pregnant women and can be toxic to people with a deficiency in glucose-6-phosphate dehydrogenase, an enzyme found in red blood cells. In developed countries, patients with P. vivax infections can be tested for the deficiency, but in developing countries, where resources are scarce, testing for the enzyme deficiency is an added economic and public health burden.
The second problem with primaquine is related to dosing. Like an antibiotic, it needs to be taken for seven to 14 days, even if the symptoms of infection are gone. “You try to get somebody to take a seven-day drug when they no longer feel sick! We don’t manage to do that,” says Mueller. He adds that a drug being developed, tafenoquine (an analog to primaquine), needs to be taken for only a couple of days. But it still doesn’t get around the problem of the patients who have the enzyme deficiency.
With the current limited arsenal of drugs, a country like Mexico faces the following scenario: “In the last six or seven years, we haven’t had any falciparum cases. But what remains is Plasmodium vivax,” says Rodriguez-Lopez, because the dormant liver form eludes treatment and keeps spreading.
Malaria eradication efforts in the 20th century focused on killing mosquitoes to stop the transmission. In Africa, P. falciparum is transmitted mainly through the mosquito Anopheles gambaie. But going after just the mosquitoes has proved to be ineffective. There are 500 known Anopheles species; to date, 40 of them have been studied, and all 40 carry Plasmodium. Even though it has a penchant for Anopheles gambaie, P. falciparum lets other Anopheles mosquitoes carry it. P. vivax appears to be even more promiscuous and can be carried by several mosquito species. Going after all Anopheles mosquitoes would be akin to herding cats.
One angle researchers, including Dinglasan at Johns Hopkins, have taken with vaccine development is to block the transmission of P. vivax. He and his group have been searching for ligands in the microvilli of the mosquito midgut, where the parasite stays during one part of its lifecycle. They identified a protein called alanyl aminopeptidase N and are pursuing it as a vaccine antigen to prevent transmission broadly, irrespective of the mosquito or parasite species. The idea is to immunize people with alanyl aminopeptidase N so that they develop antibodies against the molecule. When the mosquito sucks up blood from these immunized people, the blood will contain those N antibodies, which will interfere with the parasite’s development in the mosquito midgut.
But Dinglasan and others are still not sure how effective the strategy will be, because there are too many cautionary tales in malaria eradication. Already, Dinglasan says, with the vaccine his group is pursuing, they have data to show that the antibodies elicited against the antigen have different effects on the different parasites. “The molecule we’re targeting for the vaccine blocks 98 percent of the vivax parasites from invading the mosquito midgut, but there is enough variation or polymorphisms in the phenotype of invasion that they can potentially bypass” the antibodies, he says. “The same concentration of antibody blocks 100 percent of falciparum infections in mosquitoes in Cameroon, but it doesn’t block 100 percent of the vivax infections in mosquitoes in Thailand.”
Another vaccine-development approach is to exploit P. vivax’s fondness for the Duffy antigen, a membrane glycosylated protein on red blood cells that acts as a nonspecific receptor for chemokines. People missing the Duffy antigen for genetic reasons appear to be resistant to P. vivax. This is interesting, says Hall, because “the population in large parts of Africa is Duffy negative. That explains why you don’t find a lot of Plasmodium vivax in large parts of Africa.”
The parasite expresses a Duffy antigen binding protein, and this is another protein that Hall says researchers are going after in hopes of developing a vaccine. “By interfering with binding of the Duffy binding protein to the Duffy antigen, the idea is you can block invasion and possibly have a malaria vaccine against vivax,” explains Hall. “We’ll find out whether it works.” He cautions that the parasite’s invasion is a complex process that involves other antigens, so the Duffy antigen tactic may not pan out.
Outlook
If the Gates Foundation’s 2007 call for complete malaria eradication is to be achieved, malaria researchers say they have an uphill battle ahead of them in understanding the ways in which the other malarial parasites function. But Dinglasan, Rodriguez-Lopez and Mueller say it’s encouraging that funding agencies now are giving more emphasis to these parasites. And some progress is being made.
In 2012, the P. vivax genome was sequenced and shown to have more polymorphisms than that of P. falciparum. The diversity of single-nucleotide polymorphisms, for example, suggests that P. vivax is more functionally variable. The genome, says Hall, can act as a roadmap for exploring biochemical and molecular mechanisms to halt P. vivax.
But researchers focused on the disease outside of Africa insist that more needs to be done to tackle P. vivax and give the parasite the same level of attention as P. falciparum. Dinglasan says, “I am a card-carrying member of the malaria-eradication bandwagon. I clearly acknowledge that if we are ever to meet the goal of eradication, we cannot simply focus on falciparum malaria.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

