On the front line: Pandemic insight from a health care worker
Working in a hospital emergency department in the midst of a pandemic, I am learning a new routine. As COVID-19 numbers increase in Texas, our protocols get stricter. The state had more than 15,000 confirmed cases on Wednesday, according to Johns Hopkins University, and we have seen dozens at the hospital where I work. Our infectious disease team is working diligently to ensure the safety of the staff, so our protocols are changing continuously.
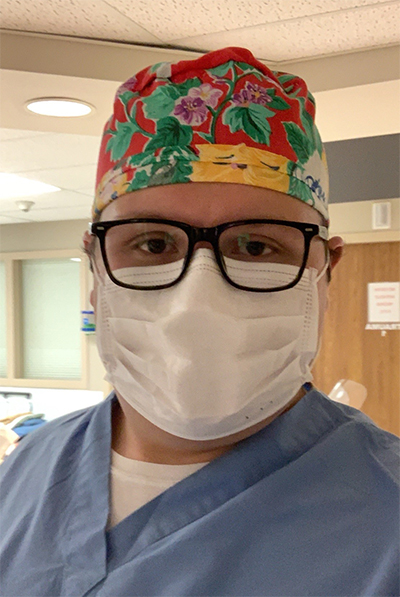
hospital, wears a scrub cap his grandmother made for him.
Before the pandemic, I got dressed at home and then drove to the hospital for my shifts as an emergency medicine technician. Now, I have to wear civilian clothes to the hospital and then change into scrubs and put on shoe covers, a surgical mask and a surgical cap. At the end of the shift, I change back into my civilian clothes and go home, strip those clothes off at the laundry, shower and put on fresh clothes. Then I am free to walk about my house. I do this to contain any potentially infectious particles I may have come into contact with.
The personal protective equipment described above is standard for interacting with any patient, whether or not they show COVID-19 symptoms. If you enter the emergency department with a toothache, you’ll see us wearing scrubs, shoe covers, caps and masks. This is for safety so we do not spread particles from our previous patients to new ones. PPE, always important, is essential during this crisis; however, faced with shortages everywhere, we are rationing our PPE gear.
When I am caring directly for a patient who shows symptoms and meets criteria for COVID-19 testing, I have to wear a gown, gloves, an N95 respirator, boot covers, shoe covers over the boot covers, goggles, a hood, a face shield and a surgical mask over the respirator. This is a lot to put on each time you enter a patient’s room.
Most health care workers share a concern about what happens when we run out of PPE: When we can no longer wear PPE with infectious patients, what do we do? Already, we get one single-use surgical mask for a 12-hour shift. That mask provides standard droplet protection. However, when we have COVID-19 patients at the hospital, we need to take precautions against both droplets and airborne particles. N95 respirators are the most secure protection against infectious particles. The hospital allots a single N95 mask for 8 hours of use. We pick and choose when we wear them, because we cannot order any more.
We have a strict no-visitor policy in the ED; all patients and staff are screened prior to entry, even patients coming in on an ambulance. The screening includes a temperature check and a questionnaire; the results determine which patients need to wear a surgical mask. Before we had the screening process, patients would grab handfuls of masks and leave with them. Each employee gets a dated sticker that we must display stating we have been screened on the current day.
As the number of patients increases, emergency departments and critical care units have become overcrowded, and we have extra staff on standby. In the month of March, I worked a total of eight shifts. In April, I am working 16 shifts to help with this influx of patients.
I sometimes feel it is a matter of “When will I contract this virus?” as opposed to “I hope I don’t contract this virus.” That’s an ominous feeling. The community has been incredibly supportive of the ED staff, sending us food and other tokens of appreciation. Though the feeling is ominous, it is reassuring knowing we have the support of our community.
In addition to working on the front line in the ED, I am a student, and the pandemic also has affected how my classmates and I learn. This semester, I am enrolled in 18 hours of coursework ranging from Biochemistry II to Calculus. It has been a struggle for students and professors to transition these intensive courses to a distanced platform and ensure the same quality of instruction. The professors have been amazing and continuously check in on us along the way. Now we have lecture videos and Zoom office hours. My main concern beyond adjusting to an online platform is my senior research. Research is an integral part of our curriculum in the chemistry department. Before spring break, I was in the purification process of important samples for my senior thesis, which had to stop.
Luckily, I am working with a sturdy protein, so my fingers are crossed that I’ll return to viable samples. Otherwise, it’s back to square one of purification.
Working increased shifts in the ED means more time away from loved ones. We have to keep our distance because we work in a high-risk environment and do not want to infect anyone. We don’t know how long this will last. I wonder sometimes when normalcy will return. Because of my work, I made the cautious decision to remain away from my family. I have not seen them in person for a couple of weeks, and I wonder when I will get to see my siblings, nieces, nephews and parents.
I look forward to the day when we can all gather around the family table for Mom and Grandma’s Southern home cooking, to laugh, play games and hug one another like we used to do. We all communicate daily via group message and the occasional phone call. This time has been especially hard on my parents, who have four children working in health care. We’ve planned a group Facetime so we can see each other. My grandmother is keeping busy by making us all scrub caps.
I am thankful for my team in the emergency department. We took an oath to put patients first and to help others. That is what we are doing, working diligently to provide the best care we can to all patients. We take risks caring for COVID-19 patients, and we make sacrifices.
This new reality has taken an emotional and physical toll on all health care workers. However, we are banded together as a community to help fight this pandemic.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Opinions
Opinions highlights or most popular articles

Women’s health cannot leave rare diseases behind
A physician living with lymphangioleiomyomatosis and a basic scientist explain why patient-driven, trial-ready research is essential to turning momentum into meaningful progress.

Making my spicy brain work for me
Researcher Reid Blanchett reflects on her journey navigating mental health struggles through graduate school. She found a new path in bioinformatics, proving that science can be flexible, forgiving and full of second chances.

The tortoise wins: How slowing down saved my Ph.D.
Graduate student Amy Bounds reflects on how slowing down in the lab not only improved her relationship with work but also made her a more productive scientist.

How pediatric cataracts shaped my scientific journey
Undergraduate student Grace Jones shares how she transformed her childhood cataract diagnosis into a scientific purpose. She explores how biochemistry can bring a clearer vision to others, and how personal history can shape discovery.

Debugging my code and teaching with ChatGPT
AI tools like ChatGPT have changed the way an assistant professor teaches and does research. But, he asserts that real growth still comes from struggle, and educators must help students use AI wisely — as scaffolds, not shortcuts.

AI in the lab: The power of smarter questions
An assistant professor discusses AI's evolution from a buzzword to a trusted research partner. It helps streamline reviews, troubleshoot code, save time and spark ideas, but its success relies on combining AI with expertise and critical thinking.

