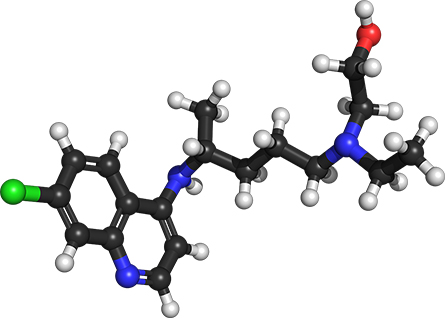
Why hydroxychloroquine and chloroquine don't block coronavirus infection of human lung cells
The big idea
A paper came out in Nature on July 22 that further underscores earlier studies that show that neither the malaria drug hydroxychloroquine nor chloroquine prevents SARS-CoV-2 – the virus that causes COVID-19 – from replicating in lung cells.
Most Americans probably remember that hydroxychloroquine became the focus of numerous clinical trials following the president’s statement that it could be a “game changer.” At the time, he appeared to base this statement on anecdotal stories, as well as a few early and very limited studies that hydroxychloroquine seemed to help patients with COVID-19 recover.
Many in the antiviral field, including myself, questioned the validity of both, and in fact, one of the papers was later disparaged by the scientific society and the editor of the journal that published it.
Since then, HQC has had a bumpy ride. It was initially approved by the FDA for emergency use. The FDA then quickly reversed its decision when numerous reports of deaths caused by heart arrhythmias emerged. That news brought many clinical trials to a halt. Regardless, some scientists continued to study it in hopes of finding a cure for this deadly virus.
How the work was done
The new study was carried out by scientists in Germany who tested HCQ on a collection of different cell types to figure out why this drug doesn’t prevent the virus from infecting humans.
Their findings clearly show that that HQC can block the coronavirus from infecting kidney cells from the African green monkey. But it does not inhibit the virus in human lung cells – the primary site of infection for the SARS-CoV-2 virus.
In order for the virus to enter a cell, it can do so by two mechanisms - one, when the SARS-CoV-2 spike protein attaches to the ACE2 receptor and inserts its genetic material into the cell. In the second mechanism, the virus is absorbed into some special compartments in cells called endosomes.
Depending on the cell type, some, like kidney cells, need an enzyme called cathepsin L for the virus to successfully infect them. In lung cells, however, an enzyme called TMPRSS2 (on the cell surface) is necessary. Cathepsin L requires an acidic environment to function and allow the virus to infect the cell, while TMPRSS2 does not.
In the green monkey kidney cells, both hydroxychloroquine and chloroquine decrease the acidity, which then disables the cathepsin L enzyme, blocking the virus from infecting the monkey cells. In human lung cells, which have very low levels of cathepsin L enzyme, the virus uses the enzyme TMPRSS2 to enter the cell. But because that enzyme is not controlled by acidity, neither HCQ and CQ can block the SARS-CoV-2 from infecting the lungs or stop the virus from replicating.
Why it matters
This matters for several reasons. One, much time and money has been spent studying a drug that many scientists said from the very beginning was not going to be effective in killing the virus.
The second reason is that the studies that have reported antiviral activity for hydroxychloroquine were not in epithelial lung cells. Thus, their results are not relevant to properly studying SARS-CoV-2 infections in humans.
What’s next?
As scientists proceed with investigating new drugs as well as trying to repurpose old ones, like hydroxychloroquine, it is critical that researchers take the time to think about their study design.
In short, those of us involved in antiviral drug development should all take a lesson from this study. It is important not only to focus our efforts on pursuing drugs that will directly shut down viral replication, but also to study the virus in the primary site of infection.![]()
The Research Brief is a short take about interesting academic work.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

