Maybe coronavirus' aggressiveness could be changed by adding
or subtracting sugar molecules
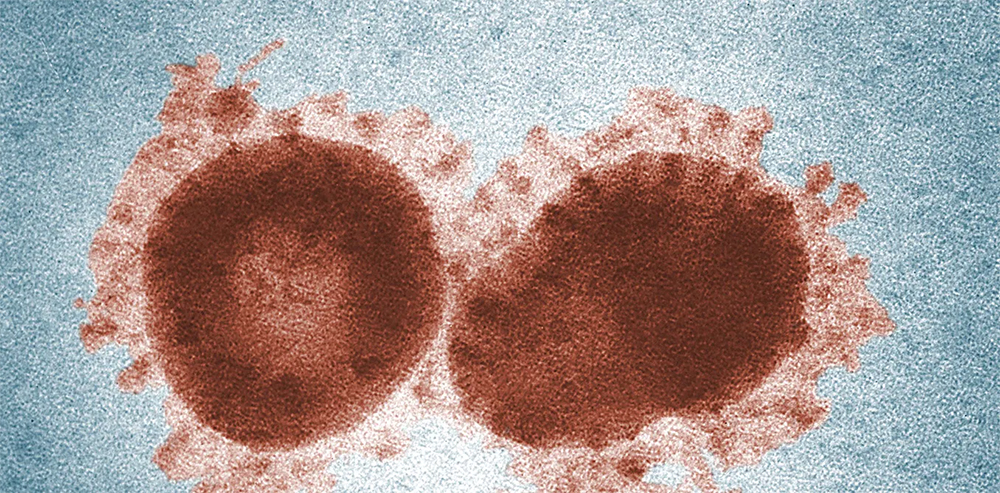
Scientists have been tracking changes to the genetic makeup of the new coronavirus to better understand how best to slow its spread. My research on the link between high blood sugar in patients and severity of illness from the virus could provide insight into the nature of different possible types of virus. Specifically, the presence of sugar on the virus’s spike protein could help differentiate them.
Many physicians noticed that people with high blood sugar, not only those with a history of diabetes but also unexplained new diabetes, were showing up in the hospital with the novel coronavirus. This indicated to me that something could be going on with the addition of sugar molecules to the virus, or the receptor it latches onto to infect cells, that influenced the severity of the disease.
I am a medical oncologist at the University of Pittsburgh who treats women with breast cancer. Colleagues of mine at the University of Pennsylvania have trials where we use the drug hydroxychloroqine to try to keep breast cancer from growing in the bone marrow, only to regrow years later. We call this tumor dormancy.
It turns out that among other things, hydroxychloroquine can serve as an oral hypoglycemic agent, lowering blood sugar.
This led me to hypothesize that the severity of novel coronavirus disease could, in part, be explained by adding of sugar molecules to the coat of the virus and its receptor.
I was therefore very interested in finding out whether there were mutations in the virus that possibly added or subtracted sugar molecules from the virus proteins, and therefore possibly either increased or decreased the severity of disease.
Sequencing novel coronavirus and scanning for mutation
Unlike prior pandemics, we have a new and very powerful tool in 2020. We are able to obtain the RNA sequence of the virus almost in real time, and track the changes in the virus as it moves from place to place.
These coronaviruses do mutate quite a bit. A group of dedicated scientists who are members of a research organization called GISAID have been doing this, and another group called Nextstrain has created a website to allow the public to see the mutations in real time. It is open source, meaning anyone can use it.
What I found (like many others) when looking through this database was that there appeared to be a common mutation in the the now well-recognized spikes that cover the surface of the virus.. The virus has specific areas where sugar is added when it replicates in cells, and the mutation appeared to increase the likelihood that a sugar molecule would be added to one of these areas. Similar mutations in other coronavirus spike proteins affected the ability of those viruses to fuse with cells.
What was interesting was that this mutation, called D614G, seemed to be more common on the East Coast of the United States than on the West Coast, and the disease seemed to be more severe on the East Coast.

While a causal link between this mutation and more severe disease remains to be proven, this may explain at least part of the difference between the severity of infections on the East and West coasts. A group in China recently found that changes in the spike protein among other mutations of the novel coronavirus taken from various people infected in Wuhan can alter the aggressiveness of the virus in cells grown in the lab. For example, strains of the novel coronavirus in Wuhan that were more similar to those in Washington and California were less aggressive in cell culture than those that were more similar to Europe.
While only a theory, this could mean that the novel coronavirus is trying out various strategies to try to live with us. If a virus is too aggressive, it may burn out too quickly by putting too many people in the hospital so it cannot spread. The milder form of the virus could spread more, and provide more immunity. Therefore, the novel coronavirus could be losing aggressiveness at it continues to move among us. This clearly is crucial to know, and needs to be tested.
Many scientists around the world are trying to figure this out. It’s interesting what a clinical observation can lead to.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

