Environmental DNA and COVID-19
Imagine discovering an animal species you thought had gone extinct was still living – without laying eyes on it. Such was the case with the Brazilian frog species Megaelosia bocainensis, whose complete disappearance in 1968 led scientists to believe it had become extinct. But through a novel genetic detection technique, it was rediscovered in 2020.

Such discoveries are now possible thanks to a new approach that recovers and reads the trace amounts of DNA released into the environment by animals. It's called environmental DNA, or eDNA – and it takes advantage of the fact that every animal sheds DNA into its environment via skin, hair, scales, feces or bodily fluids as it moves through the world.
As wildlife biologists at the University of Florida's Whitney Laboratory for Marine Bioscience & Sea Turtle Hospital, we use eDNA to track a virus responsible for a sea turtle pandemic called fibropapillomatosis, which causes debilitating tumors. We also use eDNA to detect sea turtles in the wild.
But in 2020, human health researchers began repurposing eDNA techniques to track the COVID-19 pandemic. This is a prime example of how research in one area – wildlife conservation – can be adapted to another area – human disease mitigation. Going forward, we believe eDNA will prove to be an essential tool for monitoring both human and animal health.
From soil microbes to sea turtles
Scientists in the 1980s began hunting for microbe DNA in soil samples. Over the next 20 years, the technique was adapted for use with air and water samples, and scientists started using eDNA to detect larger animals and plants.
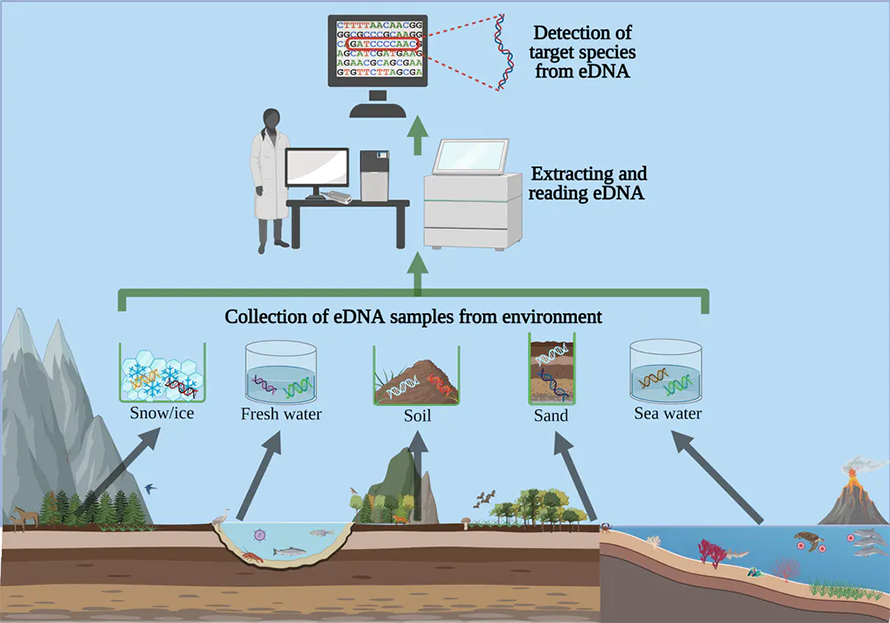
While the science behind eDNA techniques is complex, the actual process of collecting and testing a sample is relatively simple. Samples are filtered through very fine paper, which traps loose cells and strands of DNA. The techniques to read what DNA is present are the same as those used for tissue or blood samples, usually quantitative polymerase chain reaction or whole genome sequencing. Scientists can either read all of the DNA present from every organism – or target just the DNA from species of interest.
Scientists now routinely use eDNA to detect endangered wildlife and invasive species. The ability to tell whether an animal is present without ever needing to lay eyes or a lens on it is an incredible leap forward, decreasing the time, resources and human effort needed to monitor and protect vulnerable species.

However, to truly protect endangered species, it's not just the animals that need to be monitored, but the pathogens that threaten their survival. Environmental DNA is able to monitor the parasites, fungi and viruses that can cause disease in wildlife.
Tracking COVID-19
While scientists originally applied eDNA to human pathogen detection over a decade ago, it wasn't until the beginning of the current COVID-19 human pandemic that the repurposing of eDNA took off on a large scale, allowing the technology to make staggering advancements in very short order.
Coronavirus genomes consist not of DNA, but rather its cousin molecule, RNA. So researchers have rapidly optimized a variation of eDNA – eRNA – to detect coronavirus RNA in air and human wastewater.
For example, at the University of Florida Health Shands Hospital, researchers collected air samples from the hospital room of two COVID-19 patients. Using eRNA, they successfully isolated and sequenced the virus. Confirming air as a key route of transmission directly influenced public health guidelines.

When scientists apply eRNA to archived wastewater samples, the true dates of SARS-CoV-2 appearance can be detected. SARS-CoV-2 concentration in wastewater in Valencia, Spain, peaked on March 9, 2020, but the number of clinical cases didn't peak until the start of April 2020 because of the lag time between infection and severe clinical symptoms.
This sort of predictive monitoring has profound implications for health care systems, allowing time to prepare – not just for COVID-19, but for any future disease outbreaks that threaten human populations.
Intersection of diseases
It's vital that human and animal diseases are studied together. Sixty percent of emerging human pathogens come from animals – with many of these (42%) originating in wildlife populations, including Ebola, Zika, West Nile and Marburg viruses. Alternatively, people can also transmit pathogens to animals.
SARS-CoV-2 has already infected apes at a zoo in San Diego, large cats at a zoo in New York and minks at farms in Europe - the latter of which gave rise to new variants that could prove a new threat to people.
Medics, veterinarians and scientists call this convergence of human, animal and environmental well-being OneHealth or EcoHealth. Studying and treating human and wildlife disease together recognizes their commonalities and often yields breakthroughs.
With eDNA, all pathogens can be monitored in an environment regardless of where they come from. An integrated eDNA monitoring program could cost-effectively provide advanced warning of human, livestock and wildlife diseases.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
![]()
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.



