An immunologist answers three questions about COVID-19
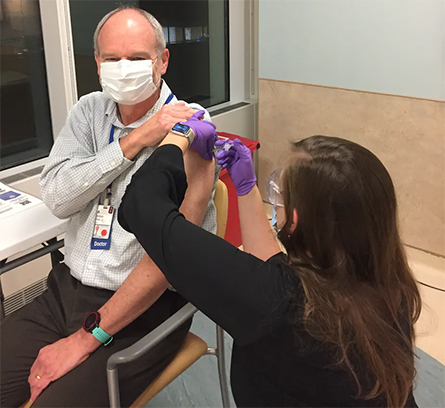
This week I was vaccinated against COVID-19 with the Pfizer mRNA vaccine, which brought to mind some frequently asked questions about the Pfizer and Moderna vaccines.
I am a professor of infectious diseases at the University of Virginia, where I care for patients with COVID-19 and conduct research on how best to prevent, diagnose and treat this new infection. As I interact with patients in the hospital, some mothers and expectant mothers have asked whether it is safe for them to take the vaccine. Here is what I have said to them.
1) Can I get vaccinated if I am pregnant or breastfeeding?
Yes, you can and should get a COVID-19 vaccine if you are either pregnant or breastfeeding.
An important reason is that COVID-19 is more severe during pregnancy. In a study of 23,000 pregnant women with symptomatic COVID-19, the Centers for Disease Control and Prevention reported pregnant women were 3 and 2.9 times more likely to end up in the ICU or on mechanical ventilation, respectively. I find it reassuring, though, that the absolute risk remains low. Only about one out of 100 pregnant women with COVID-19 is admitted to an ICU.
Vaccines are, in general, safe and well tolerated during pregnancy.
Neither the Pfizer nor Moderna COVID-19 vaccine contains the live SARS-CoV-2 virus, so there is no risk of the pregnant woman or her fetus developing COVID-19. These vaccines are safe for another reason. The mRNA used in both vaccines to stimulate a protective immune response never enters the nucleus of a cell. That means it doesn't interact with the DNA that encodes the human genome of the mother or fetus.
The caveat is that safety data is lacking for the COVID-19 vaccines, because pregnant women were intentionally excluded in the phase 3 studies of the Moderna and Pfizer vaccines.
In the absence of clinical trial data on the Pfizer and Moderna vaccines in pregnant and breastfeeding women, but with the expectation that these vaccines should be safe in these populations, both the CDC and the American College of Obstetricians and Gynecologists have recommended that vaccination be a personal decision of women who are pregnant.
For pregnant women who decide to be vaccinated, any fever associated with vaccination should be treated with acetaminophen, since fever has been associated with adverse pregnancy outcomes.
There is no concern that the vaccines will interfere with lactation and no reason not to be vaccinated if you are breastfeeding.
2) Will I be protected from asymptomatic infection?
Initial data shows 60% protection from asymptomatic infection after the first dose of the Moderna mRNA vaccine. It is likely Pfizer will also protect from asymptomatic infection, but this has not yet been shown. This means that your risk of getting an asymptomatic infection is reduced by more than half after the first dose of the Moderna vaccine.
Subjects in the phase 3 study had nasal swabs taken at the time of the second dose of the vaccine. Of these, 14 of the 15,000 volunteers in the vaccine group and 38 of 15,000 subjects in the placebo group experienced SARS-CoV-2 infection without symptoms – which is called asymptomatic COVID-19.
[Get facts about coronavirus and the latest research. Sign up for The Conversation's newsletter.]
This is evidence that asymptomatic infections are being prevented even after only the first dose. This is wonderful news, as vaccine-induced protection from asymptomatic infection will facilitate herd immunity and the end of the pandemic.
3) Will new versions of the SARS-CoV-2 virus succumb to the vaccine?
Fortunately all of the versions of the SARS-CoV-2 virus identified to date are neutralized by the COVID-19 vaccines.
The primary way that these vaccines act is by preventing the spike protein on the exterior of the coronavirus from attaching to the ACE2 protein on human cells.
The vaccines do this by triggering the human immune system to produce anti-spike antibodies that attach to the spike protein whenever they encounter it and neutralize the virus.
All 17 versions of the virus tested so far have been neutralized, including the variant that is most common in the United States.
The new variant in the United Kingdom that is likely more easily spread person to person is also unlikely to evade the new vaccines, despite the presence of mutations in the spike glycoprotein. This is in part due to the fact that there are multiple sites on the spike protein that antibodies can target to neutralize the virus. This is being formally tested now.![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

ASBMB announces 2026 JBC/Tabor awardees
The seven awardees are first authors of outstanding papers published in 2025 in the Journal of Biological Chemistry.

Missing lipid shrinks heart and lowers exercise capacity
Researchers uncovered the essential role of PLAAT1 in maintaining heart cardiolipin, mitochondrial function and energy metabolism, linking this enzyme to exercise capacity and potential cardiovascular disease pathways.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Defining JNKs: Targets for drug discovery
Roger Davis will receive the Bert and Natalie Vallee Award in Biomedical Science at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.