Fungal infections worldwide are becoming resistant to drugs and more deadly
Say “fungus” and most people in the world would probably visualize a mushroom.
But this fascinating and beautiful group of microbes has offered the world more than just foods like edible mushrooms. Fungi are also a source of antibiotics — for example, penicillin from Penicillium — as well as the yeasts and other fermentation agents that make bread rise, give cheese its flavor and put the alcohol in wine and beer.
Many people may also not realize that some fungi can cause disease. However, athlete’s foot, thrush, ringworm and other ailments are caused by fungi, and some are serious risks to health and life. That’s why the rise of antifungal resistance is a problem that needs more widespread attention — one equal to the better-recognized crises of multidrug-resistant microbes like the bacteria that cause tuberculosis.
I’ve worked in public health and medical laboratories for over three decades, specializing in public health and clinical microbiology, antimicrobial resistance and accurate science communication and health literacy. I’ve been paying close attention to the growing resistance of a pathogenic fungus called Candida auris to limited and commonly used anti-fungal agents. Since fungi have traditionally not caused major diseases, the emergence of drug-resistant fungi that can cause serious illness rarely receives funding for medical research.
But the facts suggest that this needs to change.
What’s a fungus?
Fungi-caused ailments are treated with specifically anti-fungal medications because these organisms are such a unique form of life.
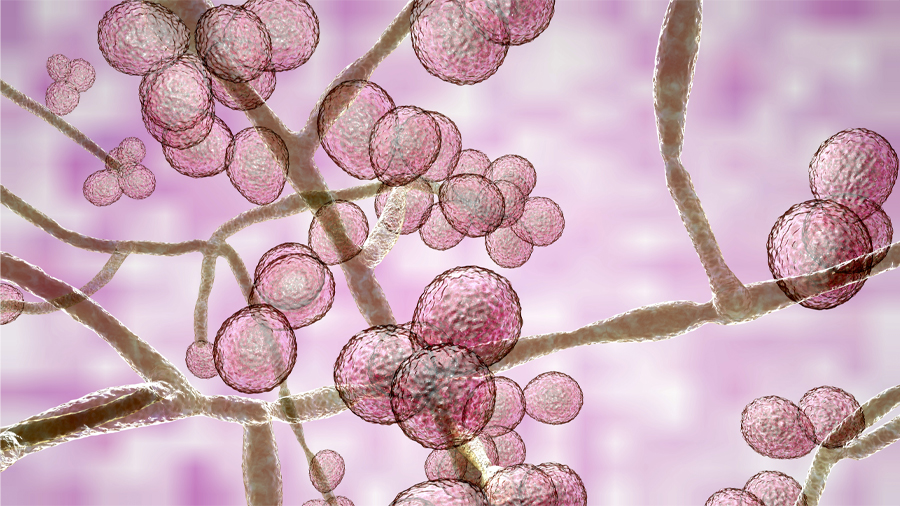
Fungi are spore-producing organisms, including molds, yeast, mushrooms and toadstools. Among their unique characteristics, fungi feed on organic matter by decomposing it, rather than ingesting it like animals do, or absorbing nutrients through roots, as plants do. Unlike bacteria, which have simple prokaryotic cells, or cells without a true nucleus, fungi have complex eukaryotic cells cells, which do have a nucleus surrounded by a membrane like animals and plants. In the multi-level taxonomy, or naming system, that biologists use to classify life forms, fungi are in their own kingdom under the domain of Eukarya.
Most fungal infections worldwide are caused by a genus of fungi called Candida, particularly the species called Candida albicans. But there are others, including Candida auris, which was first identified from an external ear canal discharge in 2009 in Japan, and given its name for the Latin term for ear, “auris.”
Candida normally lives on the skin and inside the body, such as in the mouth, throat, gut and vagina, without causing any problems. It exists as a yeast and is thought of as normal flora, or the microbes that are part of humans. Only if our bodies are immuno-compromised do these fungi become opportunistic and cause disease. That is what’s happening worldwide with multidrug-resistant C. auris.
What is the concern about Candida auris?
Infections by C. auris , sometimes called fungemia, have been reported in 30 or more countries, including the United States. They are often found in the blood, urine, sputum, ear discharge, cerebrospinal fluid and soft tissue, and occur in people of all ages. According to the U.S. Centers for Disease Control, the mortality rate in the U.S. has been reported to be between 30% to 60% in many patients who had other serious illnesses. In a 2018 overview of research to date about the global spread of the fungus, researchers estimated mortality rates of 30% to 70% in C. auris outbreaks among critically ill patients in intensive care.
Research data shows that risk factors include recent surgery, diabetes and broad-spectrum antibiotic and antifungal use. People who are immuno-compromised are at greater risk than those with healthy immune systems.
C. auris can be difficult to identify with conventional microbiological culture techniques, which leads to frequent mis-identification and under recognition. This yeast is also known for its tenacity to easily colonize the human body and environment, including medical devices. People in nursing homes and patients who have lines and tubes that go into their bodies — like breathing tubes, feeding tubes and central venous catheters — seem to be at highest risk.
The Centers for Disease Control and Prevention have set C. auris infections at an “urgent” threat level because 90% are resistant to at least one antifungal, 30% to two antifungals, and some are resistant to all three available classes of antifungals. This multidrug resistance has led to outbreaks in health care settings, especially hospitals and nursing homes, that are extremely difficult to control.
COVID-19 and C. auris: An even deadlier combination
For hospitalized COVID-19 patients, antimicrobial-resistant infections may be a particularly devastating risk of hospitalization. The mechanical ventilators often used to treat serious COVID-19 are breeding grounds and highways for entry of environmental microbes like C. auris. Further, according to a September 2020 paper authored by researchers Anuradha Chowdhary and Amit Sharma, hospitals in India treating COVID-19 have detected C. auris on surfaces including “bed rails, IV poles, beds, air conditioner ducts, windows and hospital floors.” The researchers termed the fungus a “lurking scourge” amid the COVID-19 pandemic.
The same researchers reported in a November 2020 publication that of 596 COVID-19-confirmed patients in a New Delhi ICU from April 2020 to July 2020, 420 patients required mechanical ventilation. Fifteen of these patients were infected with candidemia fungal disease and eight of those infected (53%) died. Ten of the 15 patients were infected with C. auris; six of them died (60%).
What next?
With the options for effective antifungals narrowing, the CDC is recommending a focus on stopping C. auris infections before they start. These steps include better hand hygiene and improving infection prevention and control in medical care settings, judicious and thoughtful use of antimicrobial medications, and stronger regulation limiting the over-the-counter availability of antibiotics.
In December of 2019 news emerged of a novel virus, SARS-CoV-2. Since then, most of us have been watching the terrifying headlines about the global pandemic, which has killed millions. But while we have been isolating ourselves in lockdown or quarantine, or just remaining physically distant from one another, the multidrug-resistant microbes of the world — including C. auris — have not.![]()
This article is republished from The Conversation under a Creative Commons license. Read the original article.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

