Fighting hepatitis B virus
If altruism were an organ, it would be the liver. Unless you have situs inversus, you can find yours nestled in the rib cage just beneath your right lung and diaphragm, hard at work performing more than 500 essential processes for the rest of your body.
On the one hand, the liver is a manufacturer and warehouse: It devotes itself to the manufacture of indispensable staples like albumin, clotting factors and bile. It carefully maintains stocks of vitamins and minerals — sometimes years’ worth — that it can tap into to sustain the body in times of scarcity. It stores glucose in the form of glycogen, releasing it to hungry muscles when they deplete their own stores and energizing the body during short-term starvation. During longer-term starvation, it keeps the body going by producing glucose de novo.
On the other hand, the liver is an efficient waste-management system: It retires old red blood cells and recycles their iron, filters out wayward bacteria from the bloodstream, and removes and neutralizes toxic substances such as alcohol and drugs from the blood.
But like any good superhero, the liver has its enemies. Some toxic substances such as alcohol and acetaminophen can damage it, leading to liver failure on an acute or chronic scale. A host of nefarious pathogens also target the liver, the most notorious being the hepatitis viruses: A, B, and C, plus their less-common accomplices D, E, and maybe G. All these viruses can cause acute hepatitis — or inflammation of the liver — and HBV and HCV (plus HDV, which is a satellite virus that can only replicate when HBV is around) can also cause life-threatening chronic infections that can lead to liver failure and hepatocellular carcinoma.
To mark viral Hepatitis Awareness Month this May, we’re placing the spotlight on chronic HBV, which affects 257 million people around the world and causes 60% of liver cancer cases. Dr. Hie-Won Hann, professor of medicine at Sidney Kimmel Medical College of Thomas Jefferson University, shares insights from her decades of experience working with chronic HBV patients, and Yingpu Yu, research associate in the Laboratory of Virology and Infectious Disease at The Rockefeller University, describes some recent research findings that may lead to new clinical breakthroughs.
What is HBV?
First, a quick crash course in HBV virology and pathology.
HBV is a hepatotropic virus, meaning it specifically infects hepatocytes (liver cells), which express the receptor (called NTCP) the virus recognizes to gain entry to the host cell.
Once inside, like most viruses, it gets to work converting the host cell into a factory for new viruses. The way in which it does this, however, has several features that are unique among human pathogens.
First, the partially double-stranded DNA genome of the infecting virion — in the form of “relaxed circular” DNA (rcDNA) — is converted into an extremely stable form called “covalently closed circular” DNA (cccDNA) in the nucleus of the host cell. cccDNA acts as a mini-chromosome for the transcription of viral RNAs.
The viral genome can also integrate into the hepatocyte genome, although this is not required for viral replication. In the cytoplasm of the host cell, the four viral RNAs are translated into seven viral proteins, including surface antigens of three sizes (HBsAg), core antigen (HBcAg), a secreted antigen (HBeAg), a mysterious X protein whose function is not fully understood, and—unusually—a multi-functional polymerase that includes a reverse transcriptase domain, which converts one of the RNAs into rcDNA for packing into new virions. These new virions exit the host cell, taking a bit of the HBsAg-studded cellular membrane with them as a protective (and infective) envelope, and go off to find and infect their own host hepatocytes.
All that viral replication sounds like bad news for the liver, but in fact viral replication per se doesn’t have much of a negative effect on liver function. Instead, it’s the immune system that causes damage as it attacks infected hepatocytes in an effort to destroy the virus’s strongholds. For adults who are infected for the first time with HBV, this immune response is almost always able to clear the virus from the body, often without causing any symptoms or lasting liver damage. This effective immune response prevents establishment of a chronic infection and results in the production of antibodies against the viral surface proteins that protect from future infection.
But for infants and children, it’s a different story: For reasons that are not completely understood, their immune systems are less able to fight off the virus, and 80% to 90% of infants and 30% to 50% of children progress to chronic, usually lifelong infection.
At first, the body doesn’t seem to mind its new tenant, and the virus replicates happily in the liver for many years without causing any symptoms. But then the immune system reverses its stance, deciding that the virus is no longer welcome and launching an attack on the liver.
Most patients go through several phases of immune activation that can cause progressive scarring of the liver. This can eventually result in severe, life-threatening disease such as cirrhosis and hepatocellular carcinoma, which — without treatment — occurs in about 30% of chronic HBV patients.
An unusual and dangerous feature of chronic HBV is that hepatocellular carcinoma, which usually develops only in heavily-scarred liver tissue, can emerge from an otherwise-healthy liver in as many as 50% of cases, likely because integration of the HBV genome into the host cell genome can be carcinogenic. In fact, HBV is the leading cause of liver cancer worldwide.
Who is at risk?
HBV is a blood-borne pathogen and can be transmitted by contact with infected blood and other body fluids. Because of the inverse relationship between risk of chronic infection and age, a major infection route leading to chronic infection is vertical transmission, from an infected mother to her infant during birth. Due to a combination of historic circulation patterns and low infant immunization rates, chronic HBV is most prevalent in the WHO’s South-East Asia and Western Pacific regions, which account for 60% of the 257 million cases around the world. Another 23% of chronic HBV patients live in the WHO’s Africa region. In the U.S., vaccination with a highly effective vaccine made from the viral surface antigens has been routine for all infants since 1991, helping to bring down infection rates. However, individuals who immigrate from highly affected regions remain disproportionately affected. For example, Americans of Asian and Pacific Islander heritage account for 6.8% of the total U.S. population but almost 60% of the 872,000 Americans living with chronic HBV, and up to 18% of African immigrants may be affected.
For infected individuals, there are treatments available that can slow the progression of liver disease by blocking viral replication, and periodic screening is key to identifying hepatocellular carcinoma early enough for successful treatment. However, only around 10% of people chronically infected with HBV are aware of their infection.
Identifying new patients
Dr. Hie-Won Hann has been working tirelessly for decades to bring that statistic up.
After earning her M.D. at Seoul National University Medical School (as one of just two women in her class), Hann moved to the U.S. to complete residency training and a fellowship in oncology at Harvard.

Wanting to get involved in tumor virology research, she joined Dr. Baruch Blumberg’s research group at Fox Chase Cancer Center in Philadelphia in 1971, just six years after Blumberg had discovered the HBV virus (and five before he won the Nobel Prize for the discovery). It was there that Hann’s lifelong dedication to serving patients with HBV began.
“With the approval of Dr. Blumberg’s HBV vaccine in the early 1980s, our group began HBV screening campaigns for the Asian immigrant population,” she recalled. “We visited Asian communities, mostly at churches on Sundays. After a brief lecture on HBV and liver cancer, we offered free blood testing. This allowed us to identify a large number of HBV patients and also vaccinate uninfected individuals.”
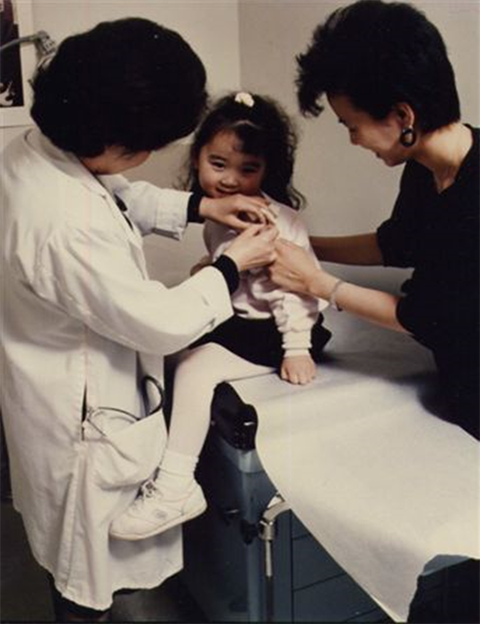
In 1988, Hann was recruited to Thomas Jefferson University Hospital to help found its Liver Disease Prevention Center. There, in addition to a full schedule seeing patients and running the Center during the week, she continued her screening efforts on Sundays along with her husband, Dr. Richard Hann, an immunologist.
“It was hard to find anyone else willing to work every Sunday!” she said.
The husband-and-wife team continued visiting churches with congregations comprised of predominantly Asian immigrants, making sure individuals their screens identified as uninfected were vaccinated and providing close monitoring for those with HBV infection.

Lifelong treatment
“There were no oral drugs available for HBV treatment until 1998,” Hann explained, so the new patients identified in her screens didn’t have many options beyond monitoring for the development of liver cancer. “Their diagnosis was striking and devastating news to them.”
So what happened in 1998 to change the outlook for chronic HBV patients?
“We at Jefferson participated in clinical trials for the first antiviral HBV drug, lamivudine. When it was approved by the FDA for HBV treatment in 1998, HBV patients finally had an effective treatment option.”
Hann subsequently participated in trials for the other four oral antivirals currently approved by the FDA for the treatment of HBV.
“Nowadays, with anti-HBV drugs available, we can reassure patients that there is effective treatment for them,” she said. “With good compliance, most patients remain well without progression to cirrhosis or liver cancer.”
Patients are typically monitored every six months for liver function, elasticity (which decreases with scarring), and hepatocellular carcinoma and begin treatment only after their immune systems start to react to the virus, which manifests clinically as elevated liver enzymes. At that point, blocking viral replication helps keep inflammation from the immune response in check so that progressive scarring is slowed.
The oral antivirals currently available for the treatment of chronic HBV all target the reverse transcriptase function of the viral polymerase, which the virus needs to synthesize the genomes of new virions. But these drugs don’t touch the cccDNA hiding out the nuclei of infected hepatocytes. That means that if therapy is stopped the virus can simply resume replication from the cccDNA templates that remain. So, to protect themselves from liver injury, patients typically have to take them for life.
For Hann, the chronicity of treatment is a major challenge in helping her chronic HBV patients stay healthy.
“Compliance is key for successful control of the virus and the disease,” she said.“Treatment is long term, and it can be costly and time consuming for busy patients to stick to. Besides, most chronic HBV patients do not have noticeable symptoms, so some don’t realize the seriousness of HBV infection,” reducing their motivation to take their medication and/or return for frequent checkups.
She added that others don’t get the care they need because they “don’t have time to visit the doctor or don’t have medical insurance.”
For Hann, the key to overcoming these challenges is clear: “We really need a curative drug.”
Research toward a cure
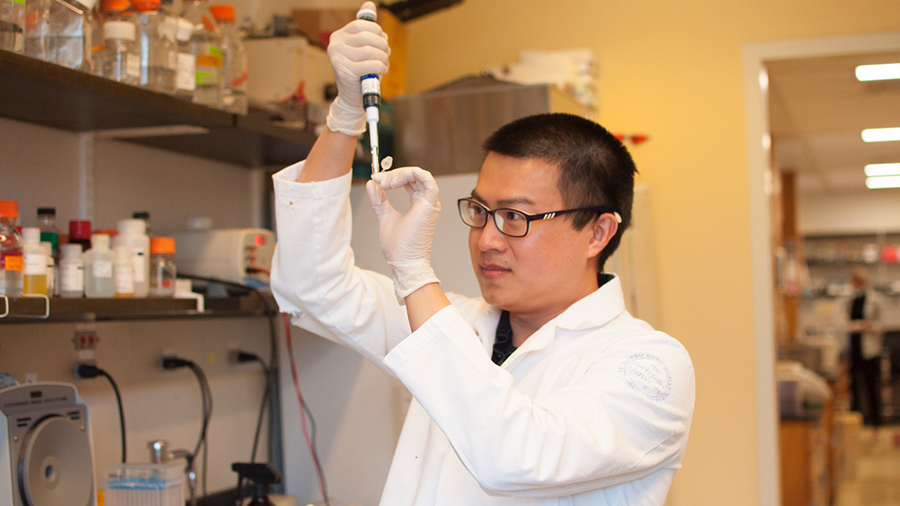
Yingpu Yu, a postdoctoral research associate studying antivirals at The Rockefeller University, agrees.
After graduating from college in his home country of China, he moved to the U.S. in 2005 to pursue a Ph.D. at SUNY Downstate Medical Center. He then joined Rockefeller in New York City to study another hepatitis virus: HCV.

Like HBV, HCV causes a chronic liver infection that can lead to serious liver disease, but it is from a completely different viral family (the Flaviviridae) and thus has little in common with HBV from a virological perspective.
During Yu’s time studying HCV, new antivirals — based on decades of basic research that established a system for studying HCV replication in the lab, elucidated the viral lifecycle to identify promising drug targets, and provided a platform for screening candidate compounds — were introduced in the clinic that raised the cure rate from around 50% to more than 95%, offering unprecedented hope for patients.
Yu’s supervisor, Charles Rice, was a co-recipient of 2020 Nobel Prize in Physiology or Medicine for his contributions to the study of HCV, which laid the groundwork for the development of these curative therapies.
Inspired by these extraordinary advances in the HCV field, Yu recently switched his research focus to HBV.
“After witnessing the incredible progress made in the treatment of HCV, I wanted to contribute to the effort to develop similarly effective treatments for HBV. I also had personal reasons that motivated me to start working on HBV: Despite progress, my country of origin, China, still has a very high rate of chronic HBV infection” — around 5% — "and several of my friends are carriers of the virus.”
To develop more effective therapeutics, Yu said, a more complete understanding of the viral lifecycle is needed.
“When we study the virus using cultured cells in the lab, we have to use a very high inoculum to establish infection. In contrast, we know from clinical observation and past studies that humans and certain animal models can become infected after exposure to a very small number of virions. This means that there are unknown factors required for efficient viral propagation that are missing from cell culture.”
Figuring out what these missing factors are not only could improve infection efficiency in vitro, allowing for development of better tools for studying viral replication and performing drug screening, but also could provide new targets for the development of novel antiviral or host-directed therapies.
Another problem is that HBV infection is difficult to model both in vitro and in vivo.
On the in vivo side, animal models — which are necessary to understand virus–host interactions, study the natural history of infection, and develop host-directed therapies — are lacking: Most common mammalian models, such as mice, are naturally insusceptible to HBV infection.
Chimpanzees are susceptible and develop a chronic infection representative of the human version; experiments in chimpanzees were instrumental in the development of the HBV vaccine and have provided a wealth of information on virus–host interactions and the immune response during HBV infection. However, for obvious reasons, they are far from a practical model, and their experimental use is limited or banned for ethical reasons in many countries.
Tree shrews, ducks, and woodchucks have also served as models (the latter two using surrogate viruses from the same family as HBV), as have mice genetically manipulated in various ways to make them permissive to infection and “humanized” mice transplanted with human liver cells, but each model comes with its own set of limitations.
An RNA launch system to study HBV
But the in vitro side is where Yu and his colleagues decided to focus their attention.
“The virus doesn’t propagate very well in cell culture. This complicates drug discovery, because initial screens for antiviral activity are usually done in cell culture. Our goal was to find a way to overcome some of the limitations inherent to existing in vitro culture methods,” he said.
Yu and fellow postdoctoral researcher Bill Schneider are first authors on a preprint, posted on the site bioRxiv, that describes their work creating a new system for initiating HBV replication in cell culture. Taking inspiration from HCV replication systems, their approach uses transfection of a single viral RNA — pregenomic RNA, or pgRNA — to launch infection.
“Background contamination is a major issue with existing methods of infection. Using viral particles to launch infection requires a high ratio of viral particles to cells; DNA and protein from the inoculum can interfere with assays to measure viral propagation. In other methods, such as transfection of HBV DNA in plasmid form and use of cell lines with the viral genome integrated into the host cell genome, most of the viral RNA and protein signal comes from the plasmid or integrated genome rather than from cccDNA, which is the template the virus uses in natural infection.”
Launching infection with pgRNA, which serves as the template for reverse transcription of the viral genome and translation of HBcAg and viral polymerase, eliminates such background contamination: In this system, all viral DNA and some viral proteins, such as HBsAg, must be the result of active replication of the virus. This not only allows for assessment of how well the virus propagates in cell culture, but also facilitates evaluation of whether a drug candidate successfully blocks viral replication.
Yu, Schneider and colleagues thought their RNA launch method might also facilitate study of drug resistance mutations, which could provide important information to guide the drug discovery process. In existing methods, viral propagation is too limited for the selection of drug-resistant mutants, and background contamination limits the detection of mutant genomes by deep sequencing.
To test their hypothesis, the team launched an infection by transfecting with pgRNA, treating infected cells with the antiviral lamivudine, and sequencing viral DNA extracted from cell supernatants. Analysis of the sequencing data revealed that two mutant genomes dominated over all other sequences, both with mutations known to confer resistance to lamivudine in patients.
“This RNA launch system expands the toolbox for dissecting the molecular mechanisms of HBV replication and interaction with hepatocytes,” said Ju-Tao Guo, a professor and chairman of the Department of Experimental Therapeutics at the Baruch S. Blumberg Institute, who was not involved in the research. “It is particularly useful in the identification of host cellular proteins involved in cccDNA intracellular amplification and regulation of cccDNA transcription. The system can also help investigate the mechanism of action of antiviral drug candidates to facilitate the development of therapeutics for the cure of chronic hepatitis B.”
“The authors describe a clever and useful technique that allows for (insights) that were not possible or practical before,” added Tim Block, president of the Hepatitis B Foundation and the Baruch S. Blumberg Institute.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

Building a career in nutrition across continents
Driven by past women in science, Kazi Sarjana Safain left Bangladesh and pursued a scientific career in the U.S.

Avoiding common figure errors in manuscript submissions
The three figure issues most often flagged during JBC’s data integrity review are background signal errors, image reuse and undeclared splicing errors. Learn how to avoid these and prevent mistakes that could impede publication.

Ragweed compound thwarts aggressive bladder and breast cancers
Scientists from the University of Michigan reveal the mechanism of action of ambrosin, a compound from ragweed, selectively attacks advanced bladder and breast cancer cells in cell-based models, highlighting its potential to treat advanced tumors.

Lipid-lowering therapies could help treat IBD
Genetic evidence shows that drugs that reduce cholesterol or triglyceride levels can either raise or lower inflammatory bowel disease risk by altering gut microbes and immune signaling.

Key regulator of cholesterol protects against Alzheimer’s disease
A new study identifies oxysterol-binding protein-related protein 6 as a central controller of brain cholesterol balance, with protective effects against Alzheimer’s-related neurodegeneration.

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

