The toxic professor syndrome
Academic biomedical research is experiencing many existential problems as relative funding dries up. This already is resulting in serious consequences for the very fabric of American biomedical investigation, its attractiveness as a career, and its long-term viability. Established investigators are disillusioned and overwhelmed, beginning investigators are disheartened, and students are turning away from pursuing academic careers in biomedical investigation.
It is intriguing that this critical issue has not become a subject of intense national debate. One would assume that the National Institutes of Health, the National Science Foundation, the Association of American Medical Colleges and other key academic societies already would have approached this issue at a strategic level. Moreover, it seems that academic societies are stuck in the primary mode of soliciting increased funding for the NIH and the NSF from Congress, rejoicing when this happens and despairing when it does not.
It should be noted that while attempting to increase government-sponsored funding is a highly laudable goal, it nevertheless is a distinct issue from assuring that a sustainable size of the workforce can be supported by existing (and projected) funding.
Since the NIH is devoted to enhancing human health and is focused on funding research that advances our understanding of human health and disease, and since the NIH has emerged as the key funding source for biomedical investigation, it seems appropriate that they take a lead in tackling this issue. So how can we attract the NIH's attention and get it to deal with this crippling problem?
Below, we propose to capture this issue and spur its serious study by formulating a new syndrome: the toxic professor syndrome. Preliminary analysis of the pathogenesis of this syndrome utilizing simple biochemical theory suggests key nodes for intervention and for developing sustainable policy.
Symptoms
The toxic professor syndrome afflicts all levels of academic rank in biomedical research. It displays a wide range of severity, from isolated anxiety over funding to fulminant disillusion and resignation from careers in biomedical research. All subjects spend increasing time chasing funding and less time advancing research, teaching and mentoring. As this imbalance is aggravated, a toxic mood permeates the entire enterprise, with increasingly sour, antagonistic and at times offensive behavior. Moreover, this toxicity spreads to trainees who increasingly shun academic careers to avoid this toxic fate.
Etiology
The etiology, pathogenesis and treatment of this syndrome are not well studied but appear primarily to trace to a mismatch between the number of independent investigators and the funds available for sustaining a healthy steady state. The latter remains dominated by NIH extramural funding, especially R01 funding.
To be sure, the NIH and NSF are not the sole causes of the toxic professor syndrome. When NIH funds increased many years ago, there was a clear expansion at many universities. More faculty members were hired, leading to an increase in the number of grant applications. Additionally, universities required investigators to obtain increasing portions of their salaries from their direct funds. In effect, and unwittingly, the NIH has emerged as the key supporter of biomedical research as well as faculty salaries. As such, academic medicine and its administrative leaders have become increasingly dependent on the NIH for basic operation. The price has been a highly leveraged financial system, leading to stress and contributing to what is effectively unfunded or underfunded faculty.
Pathogenesis
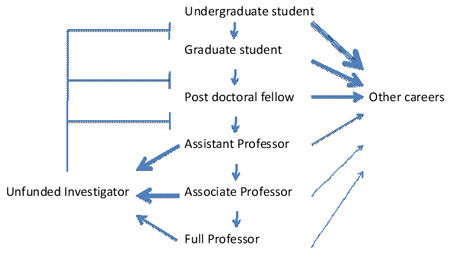
The pathogenesis of this disorder can be understood by analogy to simple metabolic pathways with a rate-limiting initial step, subsequent reactions that advance precursors/products on a metabolic pathway, and simple feedback mechanisms (Fig. 1). As flux through the pathway slows at key junctures, there is an accumulation of toxic intermediates and byproducts, primarily the unfunded investigators. This profoundly influences the operation of the system. Not only are those faculty members unable to conduct the research to which they have already committed lifetimes of study and preparation, but they become financial burdens on their departments and colleges. The professors send negative feedback signals to earlier steps in the pathway, alerting junior faculty, postdoctoral fellows, graduate students and even undergraduate students to the overflow in the system, thus discouraging students from pursuing training and careers in academic research.
Treatment
So what is the cure? The solution will entail devising a rational approach for the growth and sustainability of biomedical research as we move into the 21st century. We cannot offer specific solutions, but we do suggest some areas of study and further investigation.
One approach will require action by the NIH, preferably in conjunction with academic societies and college administrators (e.g., AAMC). From an experimental point of view, these toxic academic pathways are amenable to modeling approaches and economic analyses. For example, one could predict a reasonable steady-state number of investigators who can be supported by the system (the NIH, universities and other funding sources) and the natural turnover of those investigators, allowing the determination of a healthy rate of influx into the system. The NIH can help control the influx by awarding a predetermined number of R01s to beginning and early career investigators. The current policy of inflating this number simply backfires; it increases the flow through the assistant professor level and creates a bottleneck that spills into the unfunded investigator pathway (Fig. 1).
Academic institutions, individually or collectively (e.g., through AAMC), also could help. Lessening the salary burden on individual proposals would enhance the ability of an investigator to conduct research with a reduced number of awards. Analysis should also extend to defining the necessary size of the workforce and supplemental components as well as approaches that incentivize academic institutions to participate in defining sustainability.
There are additional examples of efforts to alleviate, if not cure, this syndrome. The American Society for Biochemistry and Molecular Biology Public Affairs Advisory Committee has outlined a series of recommendations for providing a healthier environment. These essentially involve refocusing NIH priorities toward individual-investigator, RO1-driven research.
The syndrome often affects some tissues (disciplines) more than others. As interest in basic research declines in favor of translational or big science research, some tissues suffer from a lack of support. Additionally, investigators often find their research takes them into areas where their fields historically have been unappreciated. In our field, lipid researchers have found that as they venture into areas where the importance of lipid research has not been recognized, finding expert review on study sections becomes difficult. The ASBMB Lipid Research Division is working with NIH administrators more fully to understand this aspect and provide researchers with a cadre of eligible, mid- to senior-level investigators who are willing to sit on various study sections.
The above solutions depend on organizational interventions. Clearly, members of the community must help alleviate this syndrome through active participation and prodding of action at all levels (within departments and academic centers, through representative societies, and by voicing studied opinions in national forums).
In conclusion, by presenting the current crisis in biomedical research as a syndrome approaching epidemic proportion, it is hoped that it becomes the subject of serious study and analysis. Collective and individual efforts are required. This should, in turn, stimulate innovative and exciting insights – and eventually cures – for this pervasive syndrome.
Enjoy reading ASBMB Today?
Become a member to receive the print edition four times a year and the digital edition monthly.
Learn moreFeatured jobs
from the ASBMB career center
Get the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Careers
Careers highlights or most popular articles

From humble beginnings to unlocking lysosomal secrets
Monther Abu–Remaileh will receive the ASBMB’s 2026 Walter A. Shaw Young Investigator Award in Lipid Research at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Chemistry meets biology to thwart parasites
Margaret Phillips will receive the Alice and C. C. Wang Award in Molecular Parasitology at the ASBMB Annual Meeting, March 7-10 in Washington, D.C.

Decoding how bacteria flip host’s molecular switches
Kim Orth will receive the Earl and Thressa Stadtman Distinguished Scientists Award at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Defining JNKs: Targets for drug discovery
Roger Davis will receive the Bert and Natalie Vallee Award in Biomedical Science at the ASBMB Annual Meeting, March 7–10, just outside of Washington, D.C.

Upcoming opportunities
No matter where you are in your career and what future path you aspire to, everyone needs leadership skills. Join ASBMB for practical strategies for building and practicing leadership skills.

Close out ASBMB 2026 with a bang
The closing reception of the 2026 ASBMB Annual Meeting will be held at the Torpedo Factory Art Center in Alexandra, Virginia.


