A genetic light switch for obesity lurks in the liver
Obesity is a growing problem around the world, and scientists have found that it can be caused by a variety of environmental, lifestyle and genetic factors. Age seems to be a major contributor to obesity, causing a decline in liver function and progressive adiposity through mechanisms that researchers do not yet completely understand.
Age-induced obesity in humans is likely caused by our species’ long history of food insufficiency and shorter life expectancy before advanced medicine was developed, as our ancestors’ bodies worked to create an efficient metabolism and minimize energy expenditure. However, now that people live longer and food is more plentiful in most parts of the world, these innate survival tactics are no longer helpful and may cause more harm than good.
Kamal Mehta is a professor of biological chemistry and pharmacology at the Ohio State University. Since his training with Nobel laureates Michael Brown and Joseph Goldstein at the University of Texas Southwestern Medical Center, he has dedicated his research to finding the biological mechanisms behind age- and diet-induced metabolic diseases.
“I was interested in signaling pathways regulating cholesterol homeostasis,” Mehta said. “By cell culture studies, we found a critical role of protein kinase C, or PKC, in cholesterol homeostasis. We pursued studies to define the specific isoform and narrowed it down to PKCβ. While studying whole-body PKCβ knockout mice, we realized that PKCβ plays a critical role in obesity syndrome.”
In 2008–2009, Mehta published his first papers in the Journal of Biological Chemistry and Hepatology about PKCβ’s involvement in lipid homeostasis. In his early research, he fed a high-fat diet to mice that had been genetically modified to lack the gene for PKCβ. He found that the mice were resistant to weight gain and protected from insulin resistance.
“Realizing that PKCβ can be critical for regulating both cholesterol and fat homeostasis felt great,” Mehta said.
However, it wasn’t clear which tissue caused this effect. To answer this, Mehta’s team created tissue-specific genetic knockouts of PKCβ and found that PKCβ in the liver is responsible.
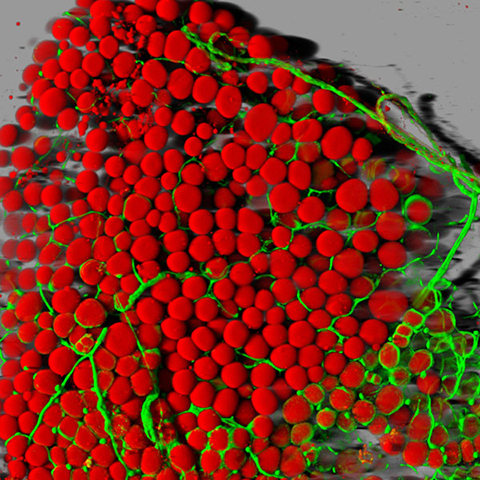
This sparked Mehta’s interest — how does PKCβ in the liver modulate other tissues? He has now answered this question. His lab’s recent paper in the JBC reported the finding that hepatic PKCβ modulates β3 adrenergic receptor, or β3-AR, signaling in the brain and peripheral tissues, which is responsible for lipolysis and thermogenesis found in brown adipose tissue, the type of body fat that regulates the body’s temperature and burns calories.
Mechanistically, age-induced activation of PKCβ can reduce the sympathetic nervous system (which is activated by metabolism) and therefore β3-AR signaling, which then decreases energy expenditure and the rate of mitochondrial oxygen consumption. This in turn leads to gradual weight gain and insulin resistance. Removing the PKCβ gene in the liver of mice reverses this effect, acting as a genetic light switch to turn off obesity.
In future studies, Mehta is interested in exploring how PKCβ regulates β3-AR signaling and how the liver communicates with the brain to achieve these effects. His lab’s findings highlight a potential avenue for drug discovery and the development of novel therapeutics for age-induced obesity; however, no PKCβ inhibitors or β3-AR agonists are currently on the market as a treatment for obesity.
“We have developed PKCβ inhibitors,” Mehta said, “and we’re pursuing further studies on utilities through my start-up Instacare Therapeutics.”
Enjoy reading ASBMB Today?
Become a member to receive the print edition monthly and the digital edition weekly.
Learn moreGet the latest from ASBMB Today
Enter your email address, and we’ll send you a weekly email with recent articles, interviews and more.
Latest in Science
Science highlights or most popular articles

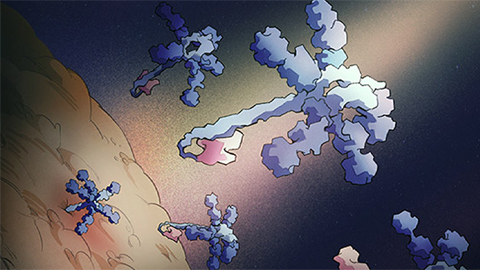
Decoding microglial language
Emory University scientists characterize extracellular vesicles that facilitate intercellular communication.

What is metabolism?
A biochemist explains how different people convert energy differently – and why that matters for your health.

What’s next in the Ozempic era?
Diabetes, weight loss and now heart health: A new family of drugs is changing the way scientists are thinking about obesity — and more uses are on the horizon.
How a gene spurs tooth development
University of Iowa researchers find a clue in a rare genetic disorder’s missing chromosome.
New class of antimicrobials discovered in soil bacteria
Scientists have mined Streptomyces for antibiotics for nearly a century, but the newly identified umbrella toxin escaped notice.
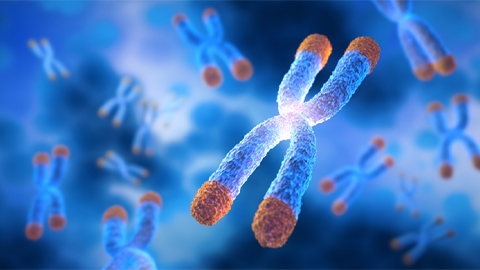
New study finds potential targets at chromosome ends for degenerative disease prevention
UC Santa Cruz inventors of nanopore sequencing hail innovative use of their revolutionary genetic-reading technique.

